How does Angina on an electrocardiogram look? Angina, a type of chest pain caused by reduced blood flow to your heart, is a common symptom of underlying cardiovascular issues. Its detection and diagnosis are very important in preventing further heart complications. One of the most widely used tools in diagnosing heart problems is the Electrocardiogram (ECG), a non-invasive test that will record the electrical activity of the heart. Let’s explore how angina presents on an ECG, its diagnostic significance, and the role ECG plays in determining the best treatment course.
What is Angina?
Angina is a medical condition characterized by chest pain or discomfort, typically caused by reduced blood flow to the heart muscle. This reduced blood flow is often due to the narrowing or blockage of the coronary arteries, a condition known as coronary artery disease (CAD). Angina can be a warning sign of more serious heart conditions, such as heart attacks or other types of cardiovascular disease.
Types of Angina
- Stable Angina: The most common form of angina, stable angina occurs with predictable patterns of chest pain or discomfort, often triggered by physical exertion or stress. It typically resolves with rest or medication, such as nitroglycerin.
- Unstable Angina: This type is more unpredictable and can occur at rest or with minimal exertion. The pain may last longer and is often more severe. Unstable angina is considered a medical emergency because it may signal an impending heart attack.
- Variant Angina (Prinzmetal’s Angina): This rare form of angina is caused by temporary spasms in your coronary arteries, leading to reduced blood flow. It often occurs at rest and is associated with specific changes in the ECG.
Causes and Risk Factors for Angina
The primary cause of angina is the narrowing or blockage of the coronary arteries due to plaque buildup (atherosclerosis). Other contributing factors include high blood pressure, high cholesterol, smoking, diabetes, stress, and a family history of heart disease. (For full details, check Angina Pectoris)
What is an Electrocardiogram (ECG)?
An Electrocardiogram (ECG) is a diagnostic tool used to measure and record the electrical activity of your heart. By attaching electrodes to your skin, an Electrocardiogram (ECG) captures the electrical impulses that trigger the heart to contract and pump blood. The test produces a graph with waves that represent different phases of the heart’s electrical cycle. These waves are labeled as the P-wave, QRS complex, and T-wave.
- P-Wave: Represents atrial depolarization (the electrical activity leading to atrial contraction).
- QRS Complex: Represents ventricular depolarization (the electrical activity leading to ventricular contraction).
- T-Wave: Represents ventricular repolarization (the process by which the ventricles recover and prepare for the next heartbeat).
How Does ECG Work?
When your heart beats, electrical impulses are generated in the sinoatrial (SA) node, located in your right atrium. These impulses travel through the heart’s conduction system, causing the atria and ventricles to contract and pump blood. The Electrocardiogram (ECG) records these electrical signals as they pass through the heart muscle, providing valuable information about heart function and rhythm.
Can Angina Be Detected on an ECG?
Angina itself does not appear directly on an Electrocardiogram (ECG), as it is a clinical symptom and not a disease. However, an ECG can reveal signs of underlying heart issues, such as ischemia (reduced blood flow to your heart), which can cause angina. For instance, changes in the ECG can indicate that a part of your heart is not receiving enough oxygen, which is a key factor in angina.
The Role of ECG in Detecting Ischemia
Ischemia occurs when the heart muscle does not receive enough oxygenated blood, typically due to blockages in the coronary arteries. During an ischemic event, the electrical signals within the heart may become altered, which can be captured on an Electrocardiogram (ECG). Therefore, while an ECG may not directly show angina, it can detect the underlying ischemic changes that cause it.
ECG in Stable vs. Unstable Angina
- Stable Angina: In stable angina, the Electrocardiogram (ECG) may not show significant abnormalities, especially when the patient is at rest. However, during an episode of chest pain or physical exertion, the ECG may show transient changes, such as ST-segment depression, which suggests temporary ischemia. These changes usually resolve once the chest pain subsides.
- Unstable Angina: Unstable angina, being more unpredictable and dangerous, may cause more prominent and persistent changes on an Electrocardiogram (ECG). The ST segment may be elevated or depressed, and T-wave inversions can occur, indicating more severe or ongoing ischemia.
Common ECG Findings Associated with Angina
Several key ECG findings are commonly associated with angina and ischemic events. These findings reflect disruptions in the heart’s electrical system due to reduced blood flow.
ST-Segment Depression

One of the most common Electrocardiogram (ECG) findings in patients with angina is ST-segment depression. The ST segment represents the period when the heart’s ventricles are contracting and pumping blood. If there is insufficient blood flow to the heart muscle, the electrical activity during this phase may be altered, leading to a downward deflection in the ST segment. This is a strong indicator of ischemia and is often seen during episodes of angina.
T-Wave Inversions
Another common Electrocardiogram (ECG) finding in angina is T-wave inversion. The T-wave represents the recovery phase of the ventricles. When the heart muscle is ischemic, this recovery phase is disrupted, causing the T-wave to invert or become more pronounced. T-wave inversions are typically seen in both stable and unstable angina.
Transient Changes During Angina Episodes
During an episode of angina, the Electrocardiogram (ECG) may show temporary changes in the ST segment or T-wave. These changes usually resolve once the chest pain subsides or the underlying ischemia is relieved. However, if the ECG abnormalities persist after the angina attack, it may indicate a more serious condition, such as a heart attack.
Limitations of ECG in Diagnosing Angina
While an Electrocardiogram (ECG) is an essential tool in diagnosing heart problems, it has certain limitations, especially when it comes to detecting angina.
False Negatives
An Electrocardiogram (ECG) may not always reveal abnormalities, especially in patients who experience stable angina with minimal or no ST-segment changes. During episodes of angina, if the ECG is not taken while the patient is experiencing chest pain, it may fail to show any signs of ischemia. This is why a normal ECG does not necessarily rule out angina.
Inability to Identify the Underlying Cause
While an ECG can indicate ischemia, it cannot pinpoint the exact cause of the reduced blood flow, such as the location or extent of coronary artery blockages. Additional tests, such as coronary angiography or stress testing, are needed to identify the underlying cause of the ischemia.
Need for Additional Tests
In some cases, a healthcare provider may need to use additional tests alongside the ECG to confirm a diagnosis of angina. Stress tests can help determine if exercise or physical exertion causes changes in the Electrocardiogram (ECG) that are consistent with ischemia. Echocardiography and coronary angiography provide further insight into the structure and blood flow in the heart, helping to confirm or rule out angina as a cause of the symptoms.
Other Diagnostic Tools for Angina
While the Electrocardiogram (ECG) is a valuable tool, it is not the only diagnostic method used to evaluate angina. Several other tests can provide more detailed information about heart health and blood flow.
Coronary Angiography
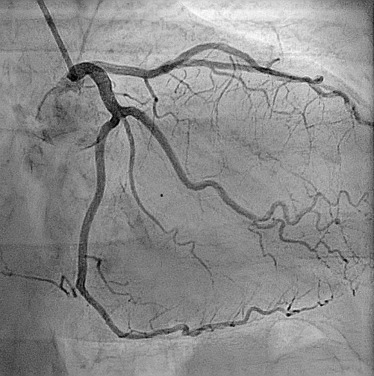
This invasive procedure involves injecting a contrast dye into the coronary arteries and taking X-ray images to visualize blockages or narrowing in the arteries. Coronary angiography provides the most accurate picture of coronary artery disease and is often used in conjunction with an ECG to confirm a diagnosis of angina.
Stress Testing
Stress testing involves monitoring the Electrocardiogram (ECG) while a patient exercises on a treadmill or stationary bike. This test helps to identify changes in the ECG that occur during physical exertion, which can indicate ischemia or angina.
Echocardiography
Echocardiography uses sound waves to create images of the heart’s chambers and blood vessels. It can help identify problems with heart function, including ischemia, and is often used to assess the severity of angina.
Clinical Relevance of ECG Findings in Angina Diagnosis
The findings from an ECG are crucial in guiding the diagnosis and treatment of angina. When a patient presents with chest pain, healthcare providers use ECG results to determine whether the pain is related to ischemia or other heart conditions.
How Healthcare Providers Interpret ECG Results
If the ECG shows ST-segment depression or T-wave inversions, the healthcare provider may suspect ischemia or angina and recommend further testing. The severity and duration of the ECG changes help determine the urgency of the situation. For example, persistent changes may indicate unstable angina, which requires immediate intervention.
The Role of ECG in Treatment Decisions
Electrocardiogram (ECG) results also play a significant role in deciding the appropriate treatment for angina. If the ECG suggests significant ischemia or an imminent heart attack, medications such as antiplatelet drugs, nitroglycerin, or beta-blockers may be prescribed. In more severe cases, procedures like angioplasty or coronary artery bypass surgery may be necessary.
Case Study Example
A 55-year-old male patient presents to the emergency room with chest pain that occurs during physical exertion. The ECG shows mild ST-segment depression and T-wave inversions. Based on the ECG findings, the physician suspects stable angina and orders a stress test and coronary angiography to assess the coronary arteries.
In conclusion, while angina itself does not directly appear on an ECG, changes in the ECG can indicate underlying ischemia that causes angina. The ECG is a valuable diagnostic tool for identifying the presence of ischemia and guiding treatment decisions. However, due to its limitations, additional tests may be required for a complete diagnosis. If you experience chest pain or other symptoms of angina, it is important to seek immediate medical attention for proper evaluation and treatment.
What People Ask Concerning ECG
Can Angina Always Be Detected on an ECG?
Not always. In some cases, the Electrocardiogram (ECG) may appear normal, especially if the patient is not experiencing angina at the time of the test. Additional tests may be required for a definitive diagnosis.
What Other Tests Are Needed if an ECG is Inconclusive for Angina?
If the ECG does not provide conclusive results, stress testing, echocardiography, or coronary angiography may be used to further assess the heart’s function and blood flow.
How Reliable is an ECG in Diagnosing Stable vs. Unstable Angina?
An Electrocardiogram (ECG) is more reliable in diagnosing unstable angina, as it often causes more pronounced and persistent changes. Stable angina may cause transient changes that may not be detected if the ECG is taken while the patient is not experiencing chest pain.
