Last updated on April 20th, 2025 at 10:58 am
What causes chest pain? Well, chest pain is caused by cardiac conditions such as angina and myocadial infation, respiatory problems, GERD, and Muscoskeletal injury. Chest pain is a symptom that can arise from a variety of causes, ranging from benign conditions like pulled chest muscle to serious and life-threatening illnesses such as heart attack.
You need to understand the potential causes of chest pain and their appropriate treatments to ensure proper evaluation, management, and timely medical intervention when needed. In this piece, you will be guided into the various symptoms, and causes of chest pain and discuss possible treatments for each.
Symptoms Associated With Chest Pain
Here is a list of common symptoms associated with chest pain that you may experience:
- Pain or discomfort in your chest: This is the primary symptom of chest pain, and it can range from mild to severe.
- Chest pressure or squeezing sensation: Chest pain may feel like a tight band around your chest or a pressure-like sensation.
- Burning or heartburn-like sensation: Some chest pain may be associated with acid reflux or indigestion.
- Sharp or stabbing pain: Chest pain can also be sharp or stabbing, and it may worsen with your movement or deep breathing.
- Radiation: The pain may radiate or spread to other areas of your body, such as the arms, neck, jaw, back, or shoulders.
- Chest discomfort with shortness of breath: Chest pain can be accompanied by chest pain-related difficulty in breathing or a feeling of breathlessness.
- Nausea and vomiting: Some people experiencing chest pain may feel nauseated or vomit.
- Cold sweats: Profuse sweating or clamminess can be a symptom of a chest cold, especially if it’s related to a heart problem.
- Lightheadedness or dizziness: Chest pain can lead you to feelings of lightheadedness or fainting.
- Fatigue: Unexplained fatigue or weakness can accompany chest pain.
- Rapid heartbeat palpitations or chest flutters: Some individuals may experience a racing or irregular heart rate along with chest pain.
- Anxiety or a sense of impending doom: Chest pain can provoke anxiety or a feeling that something is seriously wrong.
Common Causes of Chest Pain
1. Cardiac Causes of Chest Pain
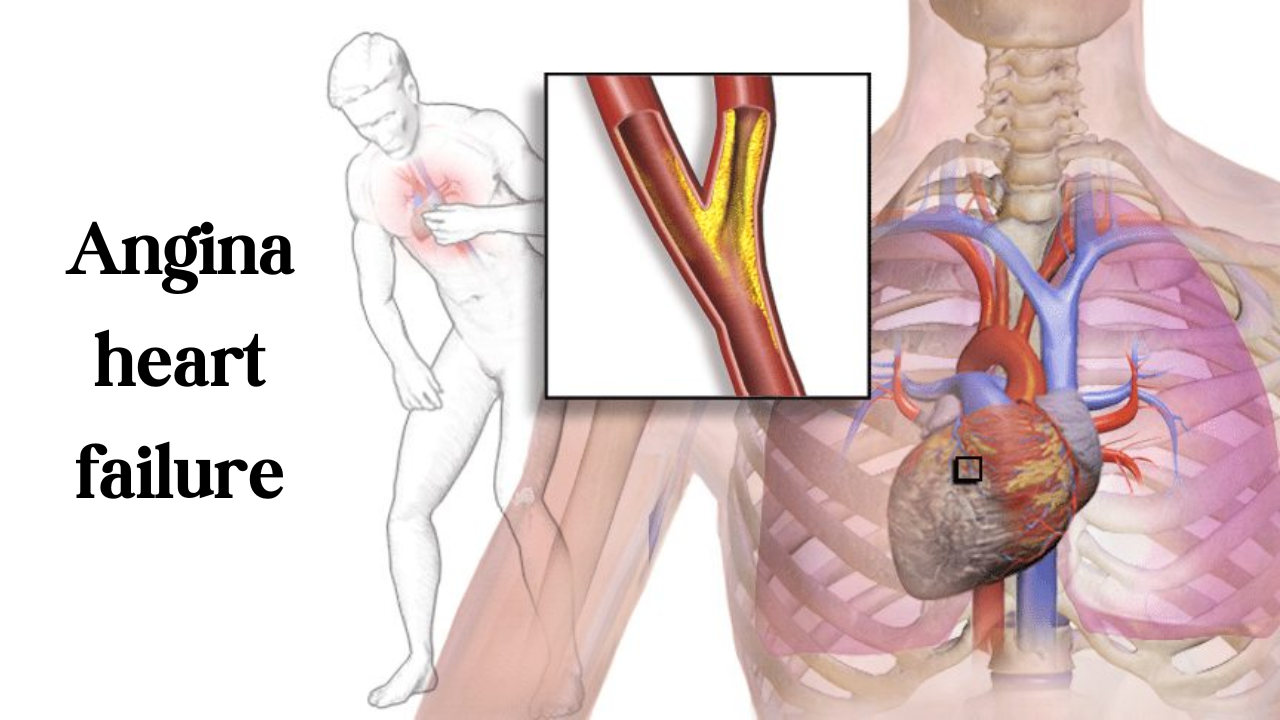
a. Angina Pectoris: Angina pectoris is chest pain or discomfort that occurs when your heart muscle doesn’t receive enough blood and oxygen due to narrowed arteries. It’s a warning sign of potential heart disease.
b. Myocardial Infarction (Heart Attack): A heart attack occurs when blood flow to a part of the heart is blocked, causing damage to the heart muscle. Chest pain during a heart attack is often severe and crushing.
2. Respiratory Causes of Chest Pain
a. Pneumonia: Chest pain can result from inflammation in the lungs due to pneumonia, often accompanied by symptoms like fever, cough, and pain when breathing.
b. Pleurisy: Pleurisy is an inflammation of the lining of the lungs and chest (pleura), causing sharp, stabbing chest pain that worsens with breathing or coughing.
3. Gastrointestinal Causes of Chest Pain
a. Gastroesophageal Reflux Disease (GERD): GERD can cause a burning sensation or discomfort in the chest (heartburn) due to stomach acid flowing back into the esophagus.
b. Peptic Ulcers: Ulcers in the stomach or duodenum can cause chest pain after eating.
4. Musculoskeletal Causes of Chest Pain
a. Muscle Strain: Chest pain can result from chest muscle pulling or injury to the chest muscles, often due to heavy lifting or physical exertion.
b. Costochondritis: Costochondritis is the inflammation of the cartilage that connects a rib to the breastbone, causing localized chest pain.
Possible Treatments for Chest Pain
There are over 20 medication for chest pain both OTC and Non-OTC drugs. Here are the categories:
1. Cardiac Chest Pain Treatments
a. Medications
- Nitroglycerin: Widely used to relieve angina by relaxing and widening the blood vessels, improving blood flow to the heart.
- Aspirin: Often administered during a heart attack to prevent further blood clotting.
b. Angioplasty and Stenting: In cases of severe blockages in the arteries, a procedure called angioplasty with stent placement can help restore blood flow to the heart.
c. Coronary Artery Bypass Grafting (CABG): This surgical procedure involves using blood vessels from other parts of the body to bypass blocked arteries in the heart.
2. Respiratory Treatments
a. Antibiotics: If chest pain is due to a bacterial lung infection like pneumonia, appropriate antibiotics are prescribed.
b. Anti-inflammatory Medications: For conditions like pleurisy, nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce inflammation and alleviate pain.
3. Gastrointestinal Treatments
a. Antacids and Acid Reducers: Antacids neutralize stomach acid, providing relief from heartburn, while acid reducers like proton pump inhibitors (PPIs) can reduce stomach acid production.
b. Lifestyle Changes: Making dietary changes (e.g., avoiding spicy foods, and caffeine), eating smaller meals, and maintaining an upright position after eating can help manage GERD.
4. Musculoskeletal Treatments
a. Pain Relievers: Over-the-counter pain relievers like acetaminophen or ibuprofen can be used to manage chest pain due to chest muscle pulling or inflammation.
b. Physical Therapy: A physical therapist can provide exercises and techniques to help alleviate chest pain caused by musculoskeletal issues.
General Tips for Chest Pain Management
- Seek Medical Attention: If you experience severe, persistent, or sudden chest pain, especially accompanied by shortness of breath and chest pressure, radiating pain, or other concerning symptoms, seek immediate medical attention.
- Regular Check-ups: Schedule regular check-ups with a healthcare professional to monitor your heart health and address any potential risk factors.
- Healthy Lifestyle: Adopt a healthy lifestyle by engaging in regular exercise, maintaining a balanced diet, managing stress, and avoiding smoking and excessive alcohol consumption.
- Know Your Risk Factors: Be aware of your risk factors for heart disease, such as high blood pressure, high cholesterol, diabetes, and a family history of heart conditions.
Frequently Asked Questions
What causes on-and-off chest pain?
Chest pain that occurs to you intermittently, or “on and off,” can result from a variety of factors. It may be due to non-cardiac causes, such as muscular strain, indigestion, or anxiety, where the pain may come and go in response to certain triggers or activities you engage in. Alternatively, cardiac conditions, like angina, can also produce episodic chest pain when the heart muscle receives insufficient blood and oxygen, typically during physical exertion or emotional stress. These fluctuations in chest pain can vary in intensity and duration, highlighting the importance of a thorough medical evaluation to determine the underlying cause and appropriate management.
What can cause pain on the right side of the chest?
Pain on the right side of the chest can be caused by a range of factors, including musculoskeletal issues like muscle strain or rib injuries, which may result from physical activity or trauma. Gallbladder problems, such as gallstones or inflammation, can manifest as right-sided chest pain, often accompanied by abdominal discomfort.
In some cases, the pain may be related to gastrointestinal issues, including acid reflux or inflammation of the esophagus. Cardiac conditions like angina or even, although less commonly, a right-sided heart attack can also cause chest pain on the right side. Given this variety of potential causes, it is essential for you to seek prompt medical attention when experiencing right-sided chest pain to determine the underlying source and appropriate treatment.
What is muscular chest pain?
Muscular chest pain is often referred to as musculoskeletal chest pain. It is a discomfort or pain that can originate from your muscles, ligaments, or tendons in the chest wall. It occurs when your chest wall structures become strained or inflamed, often due to physical overexertion, poor posture, or injury. Pulled muscle chest pain is typically localized, sharp, and worsens with movement or deep breaths. It is generally a benign condition and not related to the heart or other vital organs. Rest, gentle stretches, and anti-inflammatory medications are commonly advised by physicians to alleviate muscular chest pain, although your qualified healthcare professional should assess the pain to rule out any serious underlying issues.
What can cause chest pain besides the heart?
Chest pain can have various non-cardiac causes, including musculoskeletal issues like muscle strain, gastrointestinal problems such as acid reflux, respiratory conditions like pneumonia, and anxiety or panic attacks. These factors can lead to chest discomfort, and a comprehensive evaluation by a healthcare professional is crucial to pinpoint the exact source and determine the appropriate treatment.
What can cause burning in the chest?
Burning sensations in your chest are frequently associated with acid reflux or (GERD) which causes heartburn. Spicy or acidic foods, alcohol, or overeating can exacerbate these symptoms. More to that, anxiety and stress can lead to a burning feeling in the chest due to muscle tension and heightened sensitivity to discomfort. In some scenarios, respiratory infections or conditions like bronchitis may cause burning chest sensations, often due to inflammation and irritation in the airways.
What should I do if my lungs hurt?
Take it seriously and seek medical attention promptly. Don’t ignore persistent or severe lung pain, and if you have accompanying symptoms like shortness of breath, coughing up blood, or chest tightness, consider it an urgent matter. Consult a healthcare professional who can conduct a thorough evaluation, which may include physical exams, imaging tests, and other diagnostic procedures, to identify the source of the pain and determine the most appropriate course of action for treatment and relief. You should also try using the 8 best medicines for lung pain as prescribed to you by your physician.
What causes chest swelling?
Chest swelling-specific causes can range from benign to potentially serious. Common causes include muscular strain, injury, or inflammation of the chest wall structures. In some cases, swelling may result from localized infections, such as abscesses or cellulitis, or skin conditions like hives or contact dermatitis. More severe conditions, such as heart failure or pleural effusion, can also lead to chest swelling due to the accumulation of fluid in or around the chest cavity. Identifying the exact cause of chest swelling is crucial for appropriate diagnosis and treatment, and consulting a healthcare professional is advisable for a comprehensive evaluation.
Unexplained chest pain for years
Your unexplained chest pain that has persisted for years is a concerning medical condition that warrants your thorough investigation and evaluation. Chronic, unexplained chest pain could be due to a wide range of causes, including chronic musculoskeletal issues, gastrointestinal problems, psychological factors like anxiety or stress, or even rare conditions.
Such prolonged discomfort should not be ignored, as it may significantly affect one’s quality of life and overall health. Consultation with a healthcare professional is essential to determine the precise cause, receive appropriate diagnostic tests, and explore treatment options to alleviate chronic chest pain and improve your well-being.
What causes heartburn every day?
Some common causes of daily heartburn include:
- Diet: Certain foods and beverages can trigger heartburn in you, including spicy or acidic foods, citrus fruits, tomatoes, chocolate, caffeine, and carbonated drinks. High-fat and fried foods can also relax the lower esophageal sphincter (LES), allowing stomach acid to flow back into the esophagus.
- Obesity: Excess body weight can put pressure on the abdomen and cause the LES to relax, leading to frequent heartburn.
- Smoking: Daily smoking can weaken your LES and contribute to heartburn.
- Pregnancy: Hormonal changes during pregnancy can relax your LES and increase the risk of heartburn.
- Hiatal hernia: A hiatal hernia occurs when a portion of the stomach pushes up through the diaphragm into the chest cavity, which can contribute to heartburn.
- Medications: Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), certain blood pressure medications, and some muscle relaxers, can trigger or worsen heartburn.
- Alcohol: Excessive alcohol consumption can relax the LES and increase the risk of heartburn.
- Eating habits: Overeating, eating large meals before bedtime, or lying down immediately after eating can all contribute to you having heartburn.
- Stress and anxiety: Psychological factors can exacerbate heartburn symptoms, as stress and anxiety can increase the production of stomach acid in you.
- Underlying medical conditions: Some medical conditions, like hiatal hernias, gastroparesis, scleroderma, and connective tissue disorders, can make your heartburn more frequent.
- Delayed gastric emptying: This condition, called gastroparesis, can slow down the emptying of the stomach and increase the risk of heartburn.
- Delayed esophageal clearance: A malfunction in the esophagus that delays the movement of food and acid into the stomach can lead to persistent heartburn
How to prevent heart attack
Here are some essential and easy steps to reduce your risk of a heart attack:
- Maintain a Healthy Diet:
- Eat a balanced diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats.
- Limit your intake of saturated and trans fats, cholesterol, and sodium.
- Control portion sizes and avoid overeating.
- Minimize or avoid sugary and highly processed foods.
- Exercise Regularly:
- Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week.
- Include strength training exercises at least two days a week.
- Manage Your Weight:
- Achieve and maintain a healthy weight by balancing calorie intake with physical activity.
- Losing excess weight, especially if you are overweight or obese, can significantly reduce heart attack risk.
- Quit Smoking:
- Smoking is a major risk factor for heart disease. If you smoke, seek support to quit.
- Limit Alcohol Intake:
- If you consume alcohol, do so in moderation. Limit your intake to one drink per day for women and up to two drinks per day for men.
- Control Blood Pressure:
- Monitor your blood pressure regularly and take steps to keep it within a healthy range. This may include lifestyle changes and medication if necessary.
- Manage Cholesterol:
- Know your cholesterol levels and work with your healthcare provider to keep them within recommended ranges.
- Consider dietary changes and, if needed, cholesterol-lowering medications.
- Manage Diabetes:
- If you have diabetes, control your blood sugar levels through diet, exercise, and medication as prescribed by your healthcare provider.
- Reduce Stress:
- Find healthy ways to manage stress, such as relaxation techniques, meditation, exercise, or hobbies.
- Get Regular Check-ups:
- Visit your healthcare provider for regular check-ups to monitor your overall health and discuss heart disease risk factors.
- Follow Your Doctor’s Recommendations:
- If you have existing health conditions or take medications, follow your doctor’s advice and treatment plans.
- Be Aware of Family History:
- Know your family’s history of heart disease, as genetics can play a role. Discuss this with your healthcare provider.
- Know the Warning Signs:
- Familiarize yourself with the signs and symptoms of a heart attack (e.g., chest pain, shortness of breath, pain radiating to the arm, jaw, or back). Seek immediate medical help if you experience these symptoms.
Which condition causes inflammation and deterioration of the bone joints?
Rheumatoid arthritis (RA) is an autoimmune disease that causes chronic inflammation and joint deterioration including those in your chest. It occurs when the body’s immune system mistakenly attacks the synovium, the membranes that surround the joints. This relentless inflammation leads to joint damage, including the erosion of cartilage and bone, resulting in symptoms like joint pain, swelling, stiffness, and reduced mobility.
Without treatment, RA can lead to severe joint deformities and disability. Management typically involves a combination of medications, such as disease-modifying antirheumatic drugs and biologic agents, as well as lifestyle changes, physical therapy, and, in some cases, surgical procedures. Early diagnosis and proactive treatment are critical in preserving joint function and enhancing the quality of life for those with RA.
Final Words!
Chest pain can be caused by a range of conditions, some of which may require urgent medical attention. Understanding the potential causes and appropriate treatments is crucial for managing chest pain effectively. Always consult a healthcare professional for accurate diagnosis and tailored treatment plans to ensure the best possible outcomes and overall well-being.
Discover Substernal chest pain ICD-10