Last updated on July 11th, 2025 at 01:21 pm
In this piece, you will discover the midazolam antidote, commonly used for its mechanism, applications, and safety considerations. Learn how to manage and counteract Midazolam overdoses effectively.
What is Midazolam?
Midazolam is a powerful benzodiazepine that is widely utilized in medical settings for its sedative, anxiolytic, and anticonvulsant properties. Despite its effectiveness, there are instances where its excessive use or accidental overdose necessitates immediate medical intervention. Understanding the appropriate antidote for Midazolam, along with the mechanisms and protocols for its use, is crucial for healthcare providers and caregivers.
Midazolam is a short-acting benzodiazepine that is often administered intravenously or orally. It is commonly used for:
- Sedation during medical procedures
- Managing acute seizures
- Preoperative sedation
- Inducing anesthesia
Due to its potent effects, Midazolam must be administered with caution, particularly in individuals with underlying health conditions or those on concurrent medications.
Midazolam Overdose
Symptoms of Midazolam Overdose
Recognizing the symptoms of Midazolam overdose is critical for timely intervention. Symptoms may include:
- Extreme drowsiness
- Confusion
- Impaired motor functions
- Respiratory depression
- Hypotension
- Coma
In severe cases, Midazolam overdose can lead to life-threatening respiratory failure, requiring immediate medical attention.
Risk Factors
Several factors can increase the risk of Midazolam overdose, including:
- High dosage administration
- Concurrent use of other central nervous system depressants (e.g., alcohol, opioids)
- Existing respiratory conditions
- Advanced age
- Renal or hepatic impairment
The Commonly Used Antidote is Flumazenil
What is Flumazenil?
Flumazenil is the primary antidote used to counteract the effects of benzodiazepine overdose, including Midazolam. It is a benzodiazepine receptor antagonist that works by competitively inhibiting the binding of benzodiazepines to the GABA-A receptor.
Mechanism of Action
Flumazenil binds to the benzodiazepine receptor site on the GABA-A receptor, blocking the effects of benzodiazepines like Midazolam. This antagonistic action reverses the sedative, hypnotic, and muscle relaxant effects of Midazolam, effectively restoring normal CNS function.
Indications for Flumazenil Use
Clinical Scenarios
Flumazenil is indicated in various clinical scenarios, such as:
- Reversal of benzodiazepine sedation after medical procedures
- Management of acute benzodiazepine overdose
- Differential diagnosis of coma
Administration Protocols
Administering Flumazenil should be done under strict medical supervision. The standard administration involves:
- Initial dose: 0.2 mg intravenously over 15 seconds
- Subsequent doses: 0.2 mg every minute as needed, up to a maximum of 1 mg
The patient should be closely monitored for any adverse reactions or recurrent sedation, and additional doses may be administered based on clinical judgment.
Safety and Efficacy of Flumazenil
Efficacy
Studies have demonstrated the efficacy of Flumazenil in rapidly reversing benzodiazepine-induced sedation and respiratory depression. The onset of action is typically within 1-2 minutes, with peak effects occurring within 6-10 minutes.
Safety Considerations
While Flumazenil is generally safe, there are several considerations and potential adverse effects:
- Seizures: Particularly in patients with a history of seizure disorders or concurrent cyclic antidepressant overdose.
- Withdrawal Symptoms: Abrupt reversal of benzodiazepine effects can precipitate withdrawal symptoms in dependent individuals.
- Hypersensitivity Reactions: Rare, but possible in some individuals.
Alternative and Supportive Treatments
Supportive Care
In addition to Flumazenil, supportive care is essential in managing Midazolam overdose. This may include:
- Airway management and oxygen therapy
- Intravenous fluids to maintain blood pressure
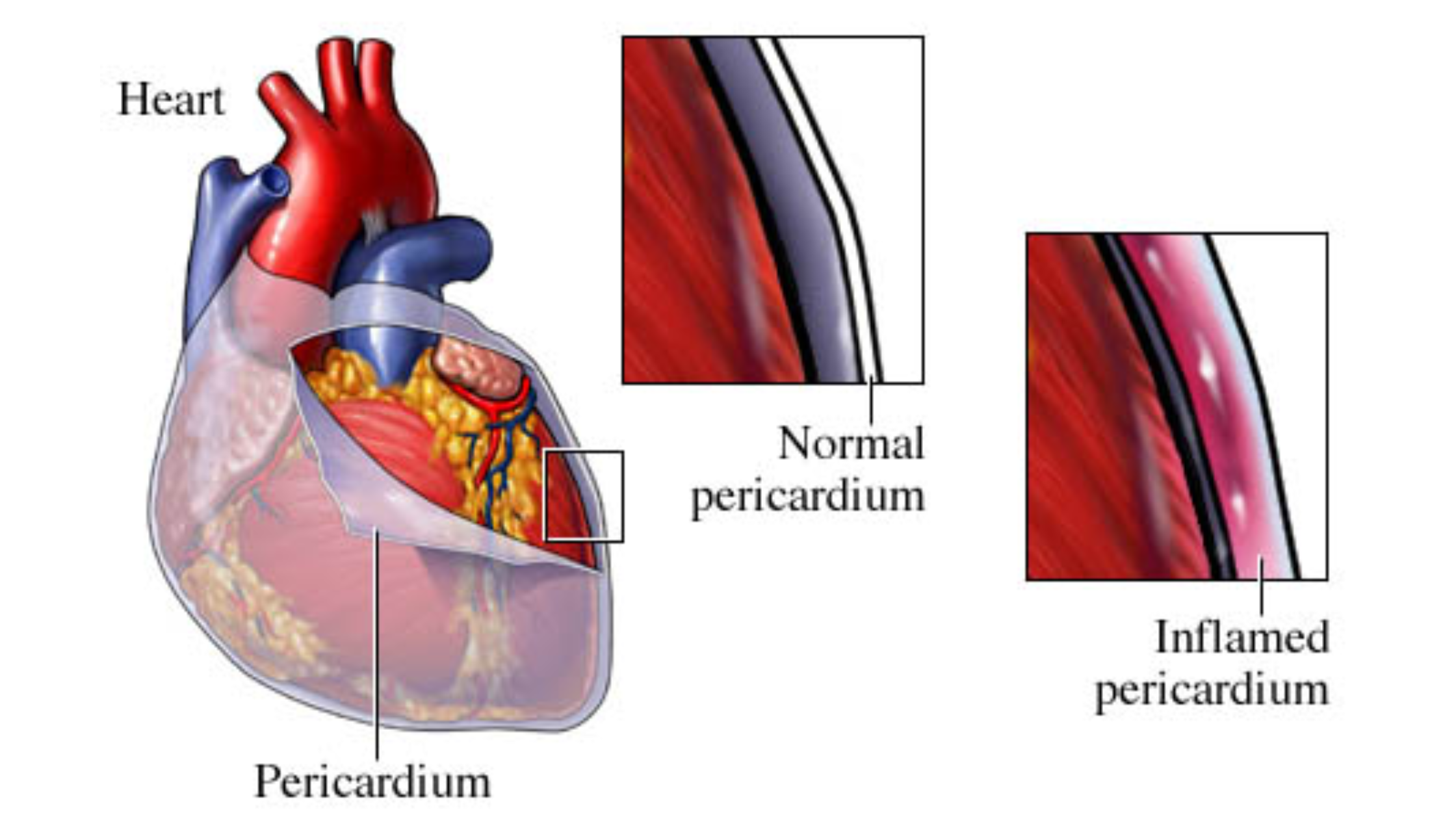
- Monitoring vital signs and cardiac function
- Symptomatic treatment of complications
Activated Charcoal
Activated charcoal may be considered if the overdose is identified early and if the ingestion is oral. It works by adsorbing the drug in the gastrointestinal tract, reducing its systemic absorption.
Prevention of Midazolam Overdose
Dosage Regulation
Proper dosage regulation and adherence to medical guidelines are crucial in preventing Midazolam overdose. Healthcare providers should:
- Carefully calculate dosages based on patient factors
- Avoid concomitant use of other CNS depressants
- Monitor patients closely during the administration
Patient Education
Educating patients and caregivers about the potential risks and signs of Midazolam overdose can help prevent accidental misuse. Important points include:
- Strictly following prescribed dosages
- Avoiding alcohol and other sedatives
- Recognizing early symptoms of overdose
Flumazenil stands as the primary antidote for Midazolam overdose, effectively reversing its sedative effects through competitive inhibition at the GABA-A receptor. Understanding the indications, administration protocols, and safety considerations of Flumazenil is crucial for healthcare providers managing benzodiazepine toxicity.
Coupled with supportive care and preventive measures, the timely use of Flumazenil can mitigate the potentially life-threatening effects of Midazolam overdose. Always consult with medical professionals for guidance and adhere to prescribed dosages to ensure the safe and effective use of Midazolam.
For more tips on managing health, visit Medical Antidote.
FAQs
1. What is the primary antidote for Midazolam overdose?
The primary antidote for Midazolam overdose is Flumazenil, a benzodiazepine receptor antagonist that reverses the effects of Midazolam.
2. How is Flumazenil administered?
Flumazenil is administered intravenously, usually in a hospital setting, with an initial dose of 0.2 mg given over 15 seconds, followed by additional doses if necessary.
3. What are the symptoms of Midazolam overdose?
Symptoms of Midazolam overdose include severe drowsiness, confusion, respiratory depression, hypotension, and, in severe cases, coma.
4. Can Midazolam overdose be prevented?
By adhering to recommended dosages, educating patients, and regular monitoring, the risk of Midazolam overdose can be minimized.
5. What supportive care is essential in managing Midazolam overdose?
Supportive care includes respiratory support, continuous monitoring of vital signs, fluid management, and, if necessary, medications to manage symptoms such as seizures or hypotension.