Last updated on May 24th, 2025 at 06:27 pm
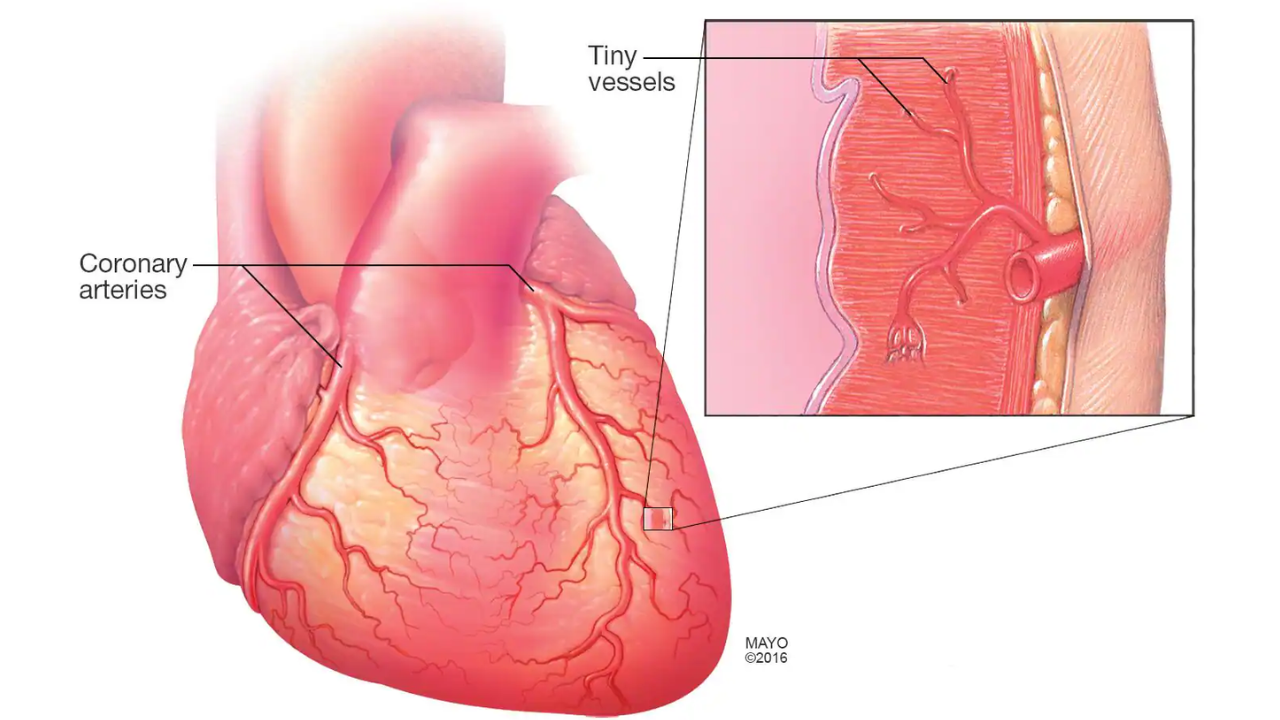
What is Microvascular Angina? Microvascular angina (MVA) is a type of chest pain caused by abnormal constriction or failure of normal dilation of the coronary resistance vessels. It is the dysfunction in the small coronary arteries, which are too small to be seen in traditional coronary angiography. Unlike typical angina, which results from blockages in large coronary arteries, MVA occurs due to impaired blood flow in the microvascular system. This condition is what was previously known as cardiac syndrome X or non-obstructive coronary artery disease (NOCAD).
Patients with MVA often experience chronic chest pain and may struggle with reduced quality of life due to frequent symptoms. Because MVA does not show up in standard angiograms, it is often underdiagnosed or misdiagnosed as anxiety, making awareness of this condition crucial.
Microvascular Angina ICD-10 Code
For medical documentation, Microvascular Angina falls under ICD-10 code I20.81, which refers to “Other forms of angina pectoris.” Since MVA is a type of angina that does not involve major artery obstruction, it is classified under this broader category.
Other related codes:
- I20.702 – Unspecified angina pectoris (sometimes used when the specific type is unclear)
- I25.1 – Atherosclerotic heart disease of native coronary artery without angina pectoris (may be relevant in some MVA cases)
Correct coding is crucial for accurate diagnosis, treatment, and insurance reimbursement.
Microvascular Angina Symptoms
MVA symptoms often mimic those of obstructive coronary artery disease (CAD), but they tend to be more persistent and unpredictable. Common symptoms include:
- Chest pain (angina) – Often described as burning, tightness, or pressure in the chest
- Pain that lasts longer than typical angina (over 10 minutes, sometimes hours)
- Pain that is not always triggered by exertion and may occur at rest
- Shortness of breath (dyspnea), even with mild activity
- Fatigue and low exercise tolerance
- Lightheadedness or dizziness
- Pain that does not respond well to nitroglycerin, a common angina treatment
MVA symptoms are frequently mistaken for anxiety, stress, or gastrointestinal issues, delaying proper diagnosis and treatment.
Microvascular Angina Testing
Since traditional angiograms do not detect small-vessel dysfunction, diagnosing MVA requires specialized testing. Common diagnostic approaches include:
1. Stress Testing (Exercise or Pharmacologic)
- Evaluates how the heart responds to stress.
- May involve treadmill exercise or medication that simulates stress on the heart.
- MVA patients may show signs of ischemia without significant large-vessel blockages.
2. Coronary Microvascular Function Tests
- Uses advanced imaging to assess blood flow in small arteries.
- Common tests include:
- Coronary flow reserve (CFR) – Measures how well small arteries dilate under stress.
- Index of Microvascular Resistance (IMR) – Evaluates small-vessel resistance.
3. Cardiac MRI or PET Scan
- Provides high-resolution imaging of blood flow.
- Helps rule out other causes of chest pain.
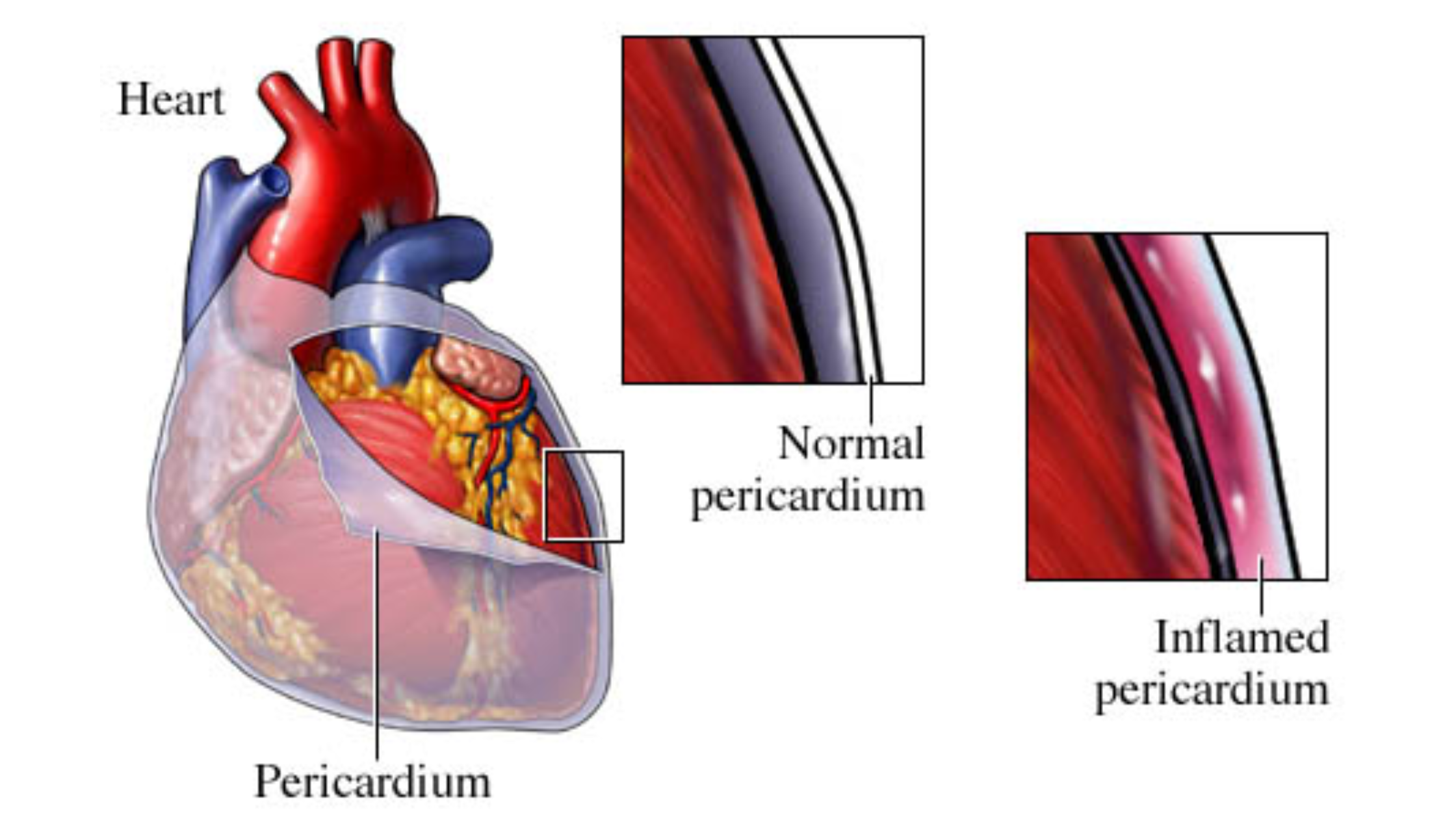
4. Endothelial Function Testing
- Assesses how well small blood vessels relax and contract.
- Abnormal results indicate microvascular dysfunction.
Early and accurate diagnosis is critical to prevent worsening symptoms and improve quality of life.
Microvascular Angina in Women
Microvascular angina is significantly more common in women, especially postmenopausal women. Studies suggest that hormonal changes, particularly estrogen decline, play a major role in the development of MVA.
Why Are Women More Affected?
- Hormonal influence: Estrogen helps maintain healthy blood vessel function. After menopause, the decline in estrogen may contribute to microvascular dysfunction.
- Atypical chest pain symptoms: Women often experience fatigue, nausea, or shortness of breath rather than classic chest pain, leading to misdiagnosis.
- Higher prevalence of inflammatory conditions: Conditions like fibromyalgia, autoimmune diseases, and metabolic syndrome are more common in women and may contribute to MVA.
- Delayed diagnosis: Women’s heart conditions are often overlooked or attributed to anxiety, delaying effective treatment.
Raising awareness about MVA in women can help prevent unnecessary suffering and improve outcomes.
Treatment of Microvascular Angina
Managing MVA requires a multifaceted approach that combines lifestyle changes, medications, and, in some cases, advanced therapies. Since traditional treatments for obstructive angina (such as stents) are ineffective, targeted microvascular angina therapy is essential.
Lifestyle Modifications
- Regular Exercise – Helps improve vascular function; low-impact activities like walking and swimming are recommended.
- Healthy Diet – A Mediterranean-style diet rich in omega-3 fatty acids, lean proteins, and fiber can improve endothelial health.
- Stress Management – Yoga, meditation, and cognitive behavioral therapy can help reduce symptoms.
- Weight Management – Reduces strain on the heart and improves overall vascular function.
- Smoking Cessation(Learn the 4 therapies to stop smoking) – Smoking worsens microvascular dysfunction and must be avoided.
Microvascular Angina Medication
Since standard angina treatments are not always effective for MVA, the following medications are commonly used:
- Beta-Blockers (e.g., Metoprolol, Carvedilol) – Improve blood vessel function and reduce chest pain episodes.
- Calcium Channel Blockers (e.g., Amlodipine, Diltiazem) – Help relax small blood vessels and improve blood flow.
- Nitrates (e.g., Nitroglycerin, Isosorbide Mononitrate) – May help some patients, but effectiveness varies.
- Ranolazine (Ranexa) – A unique anti-anginal drug that helps reduce microvascular chest pain.
- ACE Inhibitors (e.g., Lisinopril, Ramipril) – Improve endothelial function and reduce inflammation.
- Statins (e.g., Atorvastatin, Rosuvastatin) – Lower cholesterol and stabilize blood vessel function.
- Low-Dose Aspirin – This may help in some cases by improving blood flow and reducing clotting risks.
Treatment must be personalized, as not all medications work equally for every patient.
Microvascular Angina CKS (Clinical Knowledge Summaries)
The Clinical Knowledge Summaries (CKS) by NICE (National Institute for Health and Care Excellence) provide evidence-based guidelines for managing MVA. Key takeaways include:
- MVA is a real and serious condition that requires targeted treatment.
- First-line treatment includes beta-blockers, calcium channel blockers, and lifestyle changes.
- Patient education is critical to avoid unnecessary emergency visits and anxiety.
- Regular follow-ups with cardiologists specializing in non-obstructive coronary conditions improve patient outcomes.
Microvascular angina is a complex and often misunderstood condition that significantly impacts patients’ quality of life. While it primarily affects women, it can occur in anyone and requires careful diagnosis and tailored treatment.
By raising awareness and improving diagnostic techniques, healthcare professionals can help patients manage MVA effectively. If you or someone you know is experiencing unexplained chest pain, seeking a specialist in microvascular disease is crucial for proper management and relief.