Last updated on May 21st, 2025 at 08:27 am

10 lethal heart failure end-stage symptoms, what are they? Heart failure end-stage symptoms mark the most severe progression of this chronic, progressive condition, known as end-stage heart failure (ESHF). At this critical stage, the heart can no longer pump blood effectively, resulting in debilitating symptoms and a significant decline in quality of life. Understanding congestive heart failure end-stage symptoms, prognosis, and management is essential for patients, caregivers, and healthcare providers.
This research, conducted in 2025, explores the lethal aspects of end-stage heart failure, including what stage indicates symptoms of end-stage heart failure, how long end-stage heart failure lasts, and how long you can live with the final stage of heart failure. By recognizing these symptoms early, patients and families are better equipped to make informed, compassionate decisions about care priorities and available treatment options.
Congestive Heart Failure End-Stage Symptoms
Patients with end-stage heart failure experience debilitating symptoms due to the heart’s inability to pump blood efficiently. These symptoms often worsen despite optimal medical therapy. Here are the 10 lethal symptoms of end-stage heart failure:
1. Severe Shortness of Breath (Dyspnea)
- Dyspnea occurs even at rest or with minimal movement.
- Orthopnea: Difficulty breathing while lying flat, often requiring multiple pillows or sitting upright.
- Paroxysmal nocturnal dyspnea (PND): Sudden breathlessness at night, forcing the patient to sit or stand for relief.
2. Persistent Fatigue and Weakness
- Extreme tiredness due to poor oxygen delivery to muscles and organs.
- Simple activities like walking or dressing become exhausting.
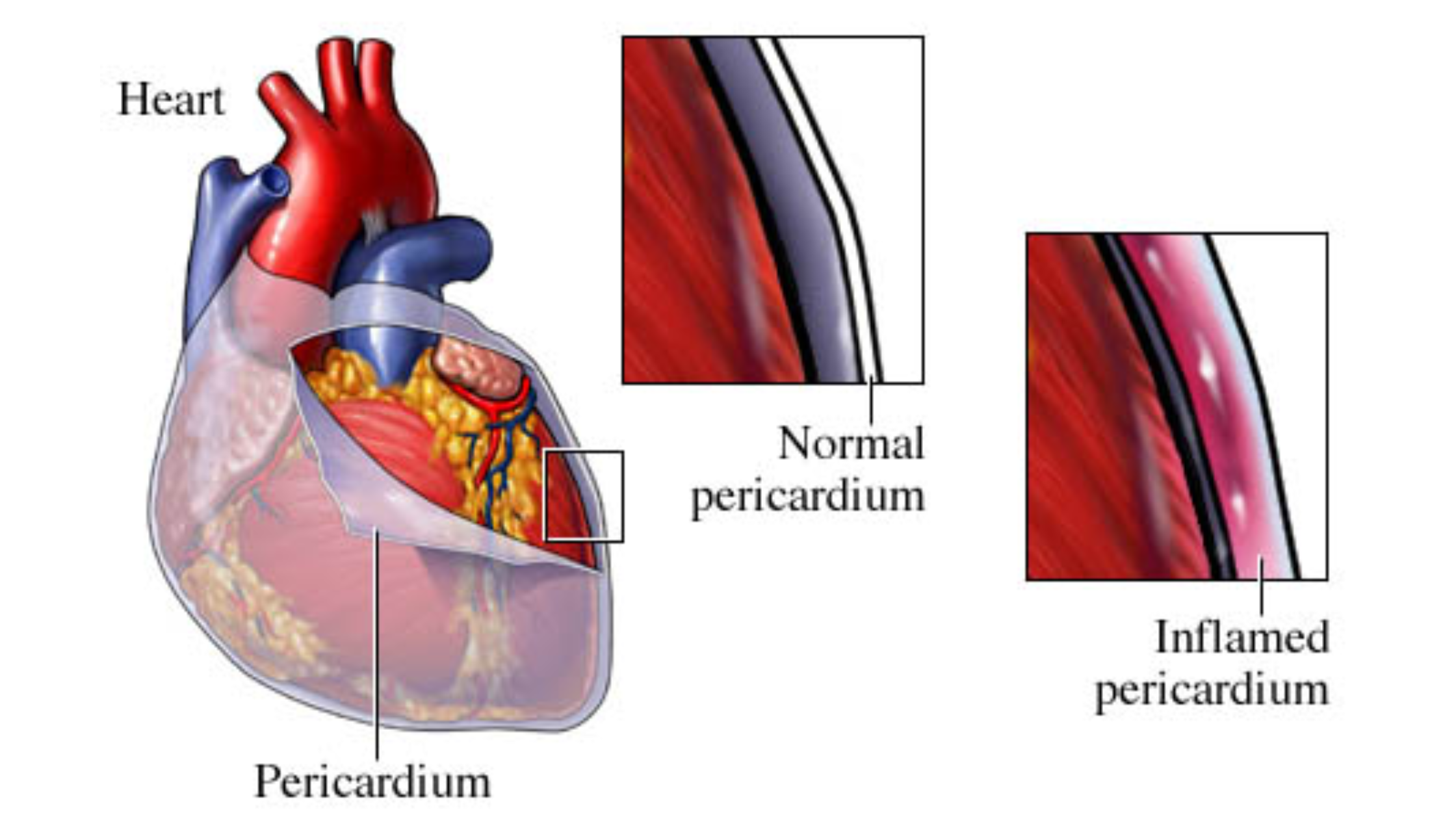
3. Fluid Retention and Swelling (Edema)
- Peripheral edema: Swelling in the legs, ankles, and feet due to fluid buildup.
- Ascites: Abdominal swelling from fluid accumulation in the peritoneal cavity.
- Pulmonary edema: Fluid in the lungs, causing severe breathing difficulties.
4. Chronic Cough or Wheezing
- Often produces frothy or pink-tinged sputum due to pulmonary congestion.
5. Rapid or Irregular Heartbeat (Arrhythmias)
- Palpitations, atrial fibrillation, or ventricular tachycardia may occur.
- Increases the risk of sudden cardiac arrest.
6. Reduced Kidney Function (Cardiorenal Syndrome)
Decreased blood flow to the kidneys leads to:
- Reduced urine output (oliguria).
- Worsening fluid retention.
- Elevated creatinine levels.
7. Cognitive Impairment and Confusion
Poor blood flow to the brain may cause:
- Memory problems.
- Disorientation.
- “Cardiac dementia” in severe cases.
8. Loss of Appetite and Nausea
- Due to poor digestion and liver congestion.
- May lead to significant weight loss (cardiac cachexia).
9. Chest Pain (Angina)
- Even without coronary artery disease, the strained heart muscle(angina pectoris) can cause discomfort.
10. Cyanosis (Bluish Skin Discoloration)
- Low oxygen levels lead to bluish lips, fingers, or toes.
What Stage Is End-Stage Heart Failure?
Heart failure is typically classified into stages based on severity, using systems like the New York Heart Association (NYHA) Functional Classification or the American College of Cardiology/American Heart Association (ACC/AHA) stages.
NYHA Classification
- Class I: No symptoms during physical activity.
- Class II: Mild symptoms with moderate exertion.
- Class III: Significant symptoms with minimal activity.
- Class IV: Severe symptoms at rest (end-stage heart failure).
ACC/AHA Stages
- Stage A: High risk but no structural heart disease.
- Stage B: Structural heart disease but no symptoms.
- Stage C: Structural disease with prior or current symptoms.
- Stage D: Refractory symptoms despite maximal medical therapy (end-stage).
End-stage heart failure (Stage D or NYHA Class IV) means the heart is severely damaged, and symptoms persist even at rest. Treatments at this stage focus on symptom relief and improving quality of life rather than curing the condition.
How Long Does End-Stage Heart Failure Last?
The duration of end-stage heart failure varies widely among patients. Factors influencing survival include:
- Underlying cause (ischemic vs. non-ischemic cardiomyopathy).
- Comorbidities (kidney disease, diabetes, COPD).
- Response to treatment (medications, devices, lifestyle changes).
- Access to advanced therapies (heart transplant, LVAD).
General Prognosis
- Without advanced interventions, 50% of patients survive for 6–12 months after diagnosis of Stage D heart failure.
- Some may live longer with aggressive management, while others deteriorate rapidly.
How Long Can You Live With Final Stage Heart Failure?
Survival in end-stage heart failure depends on multiple factors:
1. With Optimal Medical Therapy
- Diuretics, beta-blockers, ACE inhibitors, and aldosterone antagonists can prolong life but may not reverse the disease.
- Average survival: 6–12 months for most patients.
2. With Palliative Care and Hospice
- Focuses on comfort rather than cure.
- Improves quality of life but does not significantly extend survival.
3. With Advanced Interventions
- Left Ventricular Assist Device (LVAD): Can extend life by 2–5 years, but carries risks like infection and stroke.
- Heart Transplant: Offers the best long-term survival (10+ years for many recipients), but is limited by donor availability.
Factors Leading to Worse Prognosis
- Frequent hospitalizations.
- Kidney failure requiring dialysis.
- Recurrent ventricular arrhythmias.
- Inability to tolerate medications due to low blood pressure.
Management of End-Stage Heart Failure
While end-stage heart failure has no cure, treatments aim to alleviate symptoms and improve comfort.
1. Medications
- Diuretics (Furosemide): Reduce fluid overload.
- Beta-blockers (Carvedilol, Metoprolol): Slow heart rate and reduce strain.
- ACE Inhibitors/ARBs (Lisinopril, Valsartan): Improve heart function.
- Aldosterone Antagonists (Spironolactone): Reduce fluid retention.
- Inotropes (Milrinone, Dobutamine): Short-term use in severe cases.
2. Oxygen Therapy
- Helps with severe hypoxia due to pulmonary edema.
3. Lifestyle Adjustments
- Fluid and salt restriction to prevent worsening edema.
- Small, frequent meals to ease digestion.
4. Advanced Therapies
- LVAD (Left Ventricular Assist Device): Mechanical pump for the heart.
- Heart Transplant: Best option for eligible patients.
5. Palliative and Hospice Care
- Focuses on pain relief, emotional support, and improving quality of life.
End-stage symptoms of heart failure are a severe and life-limiting condition marked by debilitating congestive heart failure end-stage symptoms, including extreme shortness of breath, fatigue, and fluid retention. Recognizing the stage of end-stage heart failure aids in identifying the progression of the disease..
Prognosis varies, however, most patients have a life expectancy of 6–12 months without advanced interventions. Therapies like LVADs or transplants can extend life for some. The key question—how long can you live with final-stage heart failure?—depends on individual health, treatment response, and access to care.
Early palliative care involvement ensures symptom relief and improves the patient’s remaining quality of life. By recognizing these signs and seeking appropriate care, patients and families can make informed decisions during this challenging phase.