In this piece, you will unveil the essential information about the antidote for Tylenol overdose (Mucomyst), symptoms of acetaminophen toxicity, and effective treatment protocols.
Tylenol, known generically as acetaminophen, is one of the most commonly used over-the-counter pain relievers and fever reducers. Despite its widespread use and general safety when taken as directed, an overdose of Tylenol can lead to severe and potentially fatal liver damage. Understanding the antidote for Tylenol overdose, recognizing the symptoms of acetaminophen toxicity, and knowing the appropriate treatment options are critical for anyone who uses this medication. This comprehensive guide will delve into the essential aspects of managing Tylenol toxicity effectively, with a particular focus on Mucomyst, the primary antidote for acetaminophen overdose.
Tylenol Overdose
Symptoms of Tylenol Overdose
An overdose of Tylenol can present a range of symptoms, which typically develop in stages over time. Early symptoms of acetaminophen toxicity may include:
- Nausea and vomiting
- Abdominal pain
- Loss of appetite
- Sweating
- Pallor
As the overdose progresses, more severe symptoms can develop, such as:
- Right upper quadrant pain (indicating liver distress)
- Jaundice (yellowing of the skin and eyes)
- Confusion
- Weakness
- Bleeding or bruising easily
- Hypoglycemia (low blood sugar)
- Hepatic encephalopathy (a decline in brain function due to severe liver damage)
Recognizing these symptoms early and seeking immediate medical attention can significantly improve the outcome of a Tylenol overdose.
The Importance of Immediate Medical Attention
Tylenol overdose is a medical emergency that requires prompt intervention. If you suspect an overdose, it’s vital to seek immediate medical help. Delaying treatment can lead to severe liver damage, multi-organ failure, or even death. Timely administration of the appropriate antidote is crucial for a positive outcome.
The Antidote for Tylenol Overdose is Mucomyst
What is Mucomyst?
Mucomyst, generically known as N-acetylcysteine (NAC), is the primary antidote for tylenol overdose. It is an effective treatment that works by replenishing glutathione stores in the liver, helping to detoxify acetaminophen metabolites and prevent liver damage.
Mechanism of Action
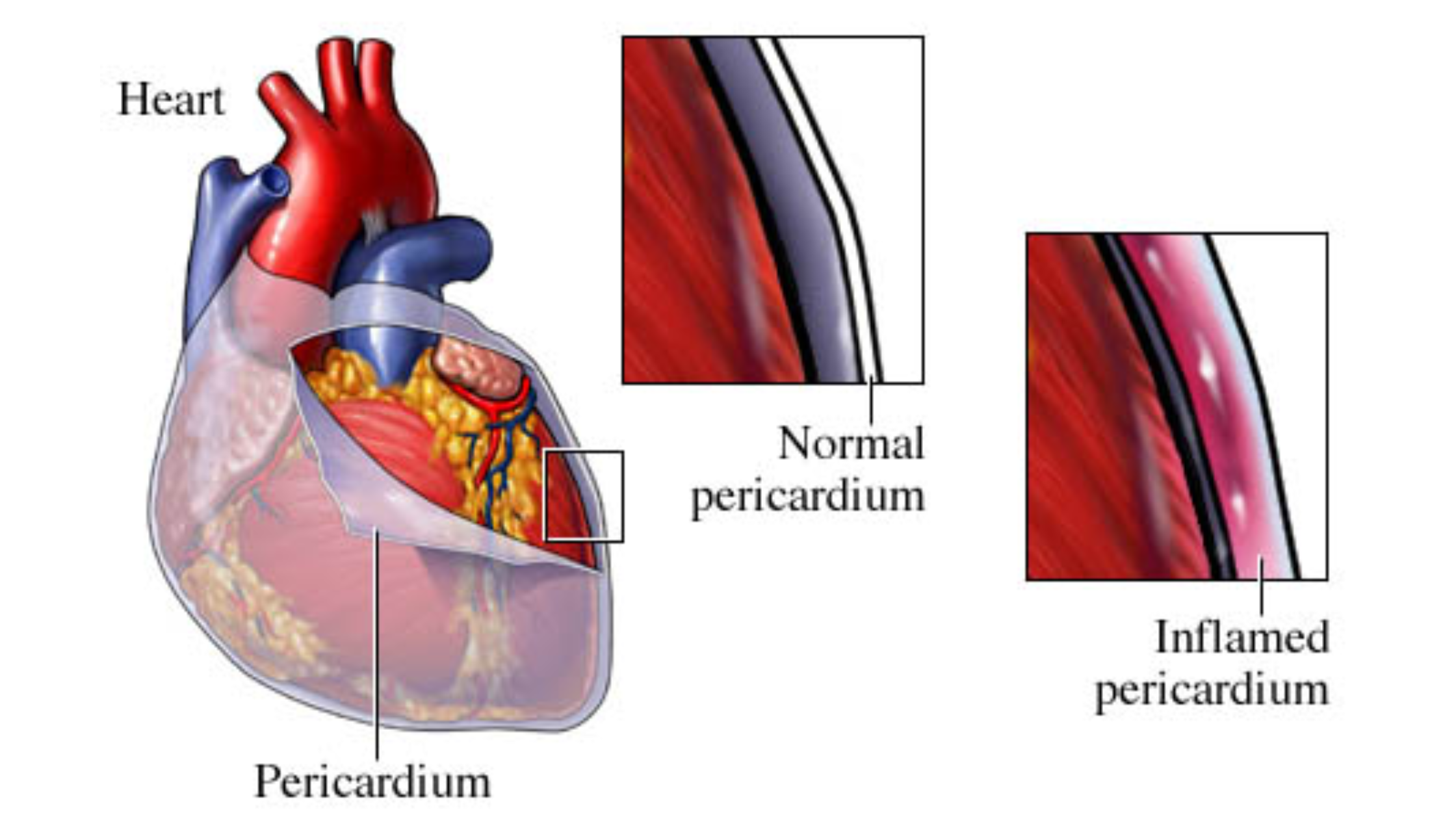
When Tylenol is ingested, it is metabolized in the liver. In cases of overdose, the liver’s ability to safely metabolize acetaminophen is overwhelmed, leading to the production of a toxic metabolite called N-acetyl-p-benzoquinone imine (NAPQI). NAPQI binds to liver cells, causing oxidative damage and cell death.
Mucomyst works by:
- Replenishing Glutathione: NAC provides a substrate for glutathione synthesis, which helps neutralize NAPQI and prevent liver damage.
- Directly Binding to NAPQI: NAC can also bind directly to NAPQI, detoxifying it and reducing its harmful effects on liver cells.
- Enhancing Sulfation: NAC promotes the sulfation pathway, which helps in the safe metabolism and excretion of acetaminophen.
Administration of Mucomyst
Mucomyst can be administered via oral or intravenous routes, depending on the severity of the overdose and the patient’s condition.
Oral Administration
Oral NAC is typically given in a specific dosing regimen over 72 hours. The dosing schedule is as follows:
- Loading Dose: 140 mg/kg of NAC orally.
- Maintenance Dose: 70 mg/kg every 4 hours for a total of 17 doses.
Intravenous Administration
Intravenous NAC is used when the patient is unable to tolerate oral administration or in cases of severe overdose. The IV dosing regimen typically lasts 21 hours:
- Loading Dose: 150 mg/kg in 200 ml of 5% dextrose over 60 minutes.
- Second Dose: 50 mg/kg in 500 ml of 5% dextrose over 4 hours.
- Third Dose: 100 mg/kg in 1000 ml of 5% dextrose over 16 hours.
Effectiveness of Mucomyst
When administered within 8-10 hours of overdose, Mucomyst is highly effective in preventing significant liver damage. Even when given later, it can still mitigate damage and improve outcomes. The key to its effectiveness lies in early detection and timely administration.
Treatment and Management of Tylenol Overdose
Initial Assessment
Upon suspecting a Tylenol overdose, a thorough initial assessment is crucial. This includes:
- History: Determine the amount of acetaminophen ingested, the time of ingestion, and any co-ingested substances.
- Physical Examination: Assess for signs of toxicity, including jaundice, liver tenderness, and mental status changes.
- Laboratory Tests: Measure serum acetaminophen levels, liver function tests (LFTs), and coagulation profiles. The Rumack-Matthew nomogram can help determine the need for NAC based on acetaminophen levels and time since ingestion.
Supportive Care
In addition to administering Mucomyst, supportive care is essential for managing Tylenol overdose:
Activated Charcoal
Activated charcoal can be administered if the overdose is detected within 1-2 hours of ingestion. It binds to acetaminophen in the gastrointestinal tract, reducing its absorption.
Intravenous Fluids
IV fluids help maintain hydration and support renal function, which is crucial for the excretion of acetaminophen and its metabolites.
Monitoring and Observation
Continuous monitoring of vital signs, liver function, and renal function is critical. Regular blood tests help track the progress of the treatment and detect any complications early.
Symptomatic Treatment
Symptomatic treatments may include:
- Antiemetics: To manage nausea and vomiting.
- Analgesics: For pain relief, avoid additional acetaminophen-containing medications.
- Electrolyte Management: To correct any imbalances caused by the overdose or its treatment.
Advanced Interventions
In severe cases where significant liver damage has occurred, more advanced interventions may be necessary:
Liver Transplantation
In cases of acute liver failure due to Tylenol overdose, liver transplantation may be the only option for survival. This is considered when the patient meets specific criteria, such as severe coagulopathy, encephalopathy, and metabolic acidosis.
Intensive Care Unit (ICU) Admission
Patients with severe toxicity and multi-organ failure require intensive care. Supportive measures in the ICU may include mechanical ventilation, vasopressors for blood pressure support, and renal replacement therapy (dialysis).
Prevention of Tylenol Overdose
Proper Dosage
Always follow the recommended dosage instructions provided by healthcare providers or as indicated on the packaging. Avoid taking multiple acetaminophen-containing products simultaneously.
Education and Awareness
Educate yourself and others about the risks of acetaminophen overdose and the importance of adhering to dosage guidelines. Be aware of the potential for acetaminophen in combination medications, such as those used for colds and flu.
Child Safety
Keep all medications, including Tylenol, out of reach of children. Use child-resistant packaging and educate older children about the dangers of medication misuse.
Regular Monitoring
For those who take acetaminophen regularly for chronic conditions, regular monitoring by healthcare providers is crucial. This includes periodic liver function tests to detect any early signs of toxicity.
Consulting Healthcare Professionals
Always consult with healthcare professionals before starting or changing any medication regimen. This is especially important for individuals with preexisting liver conditions or those taking other medications that may interact with acetaminophen.
Conclusion
Understanding the antidote for Tylenol overdose and the necessary treatment protocols can be life-saving. Recognizing the symptoms of overdose, seeking immediate medical attention, and knowing the appropriate treatments, including Mucomyst (N-acetylcysteine), are crucial steps in managing acetaminophen toxicity. Additionally, preventive measures such as adhering to prescribed dosages, educating others, and consulting healthcare professionals for guidance can help avoid the risk of overdose. Remember, responsible medication use and prompt intervention are key to maintaining health and safety.
By being well-informed and prepared, you can effectively handle a Tylenol overdose situation, ensuring the best possible outcome for yourself or a loved one. Stay safe, stay informed, and always prioritize health and well-being.
.