Last updated on April 17th, 2025 at 01:40 pm
Antidote for hyperkalemia is also called the potassium antidote. Hyperkalemia treatment includes the use of calcium gluconate and other treatments for managing high potassium levels effectively. Hyperkalemia, a condition characterized by elevated levels of potassium in your blood, is a serious medical issue that requires prompt and effective treatment.
Why the Antidote for Hyperkalemia is Necessary
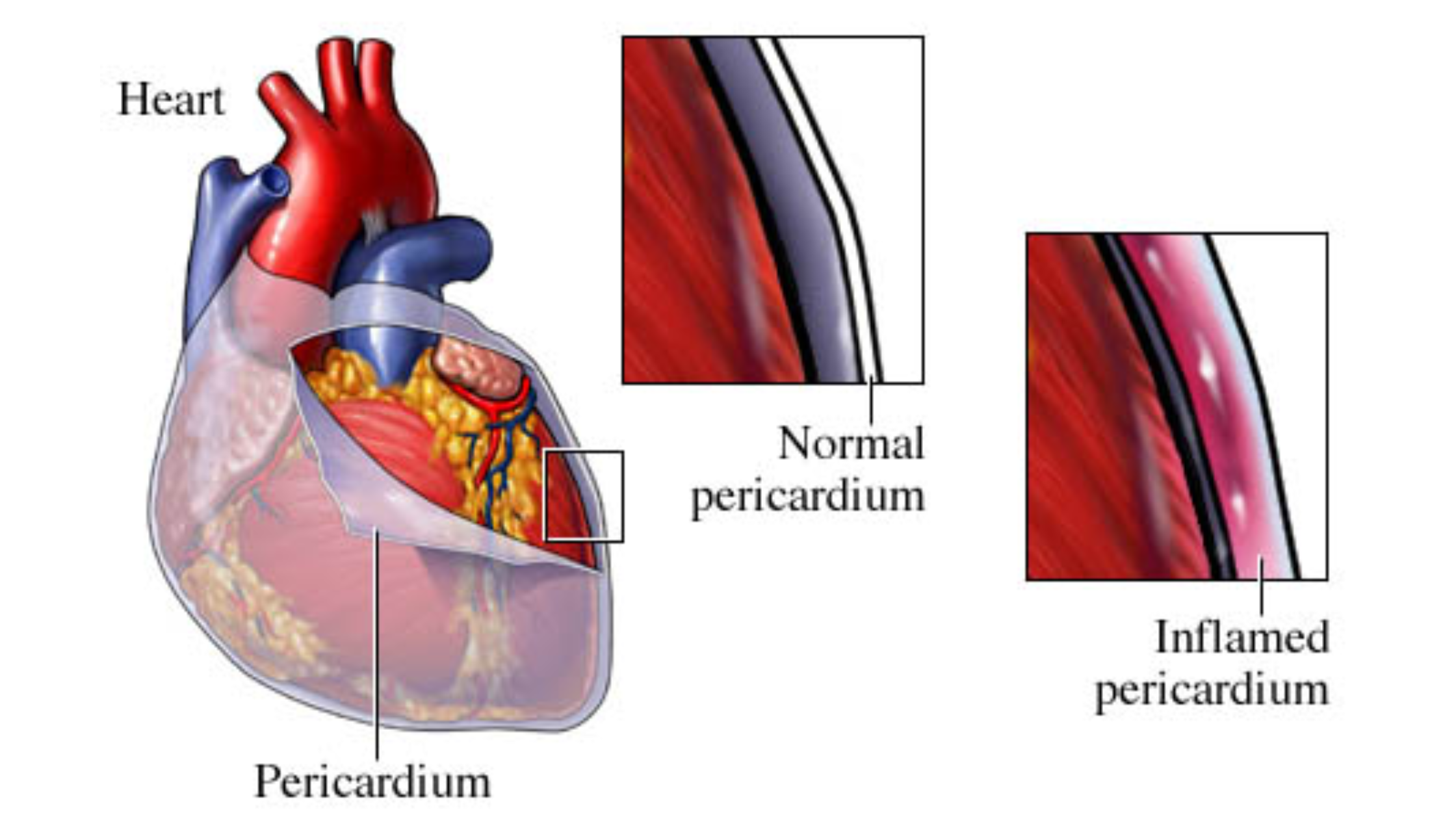
Potassium is an essential electrolyte that plays a critical role in various bodily functions, including nerve signal transmission and muscle contraction. However, too much potassium can disrupt these processes, leading to potentially life-threatening complications, especially affecting your heart. In this comprehensive guide, we will explore the antidote for hyperkalemia, focusing on calcium gluconate, treatment options, and remedies to manage high potassium levels.
What is Hyperkalemia?
Hyperkalemia refers to an abnormally high level of potassium in your blood, typically defined as a serum potassium concentration greater than 5.0 milliequivalents per liter (mEq/L). Potassium is a vital mineral found primarily inside the cells, with only a small fraction present in the bloodstream. It is crucial for maintaining the proper function of cells, nerves, and muscles, particularly the heart.
Causes of Hyperkalemia
Hyperkalemia will result from various factors, including:
- Kidney Dysfunction: The kidneys play a pivotal role in regulating potassium levels. Conditions such as chronic kidney disease (CKD) or acute kidney injury (AKI) can impair the kidneys’ ability to excrete potassium, leading to its accumulation in the blood.
- Medications: Certain medications, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), potassium-sparing diuretics, and nonsteroidal anti-inflammatory drugs (NSAIDs), can increase the risk of hyperkalemia.
- Excessive Potassium Intake: Consuming large amounts of potassium-rich foods or supplements can overwhelm the body’s ability to maintain balanced potassium levels.
- Cellular Shifts: Conditions like acidosis, hemolysis, and tissue breakdown (e.g., trauma or severe burns) can cause potassium to shift from inside the cells to the bloodstream.
- Hormonal Imbalances: Disorders such as Addison’s disease, characterized by insufficient production of aldosterone, can lead to impaired potassium excretion.
Symptoms of Hyperkalemia
Mild hyperkalemia may be asymptomatic, but severe cases can present with symptoms such as:
- Muscle weakness or paralysis
- Fatigue
- Nausea and vomiting
- Heart palpitations
- Chest pain
- Shortness of breath
- Abnormal heart rhythms (arrhythmias)
What is the Antidote for Hyperkalemia?
Treating hyperkalemia involves a combination of immediate interventions to stabilize the heart, shift potassium into the cells, and enhance its excretion from the body. The choice of treatment depends on the severity of hyperkalemia and the presence of symptoms or underlying conditions.
Immediate Interventions
- Calcium Gluconate: Calcium gluconate is often the first-line treatment in severe hyperkalemia, particularly when there are changes in the electrocardiogram (ECG) indicative of potassium’s effect on the heart. It does not lower potassium levels but stabilizes the cardiac cell membrane, reducing the risk of arrhythmias.
- Intravenous Insulin and Glucose: Insulin, usually administered with glucose to prevent hypoglycemia, helps drive potassium into the cells, temporarily reducing serum potassium levels.
- Beta-2 Agonists: Medications such as albuterol can also promote the movement of potassium into the cells.
- Sodium Bicarbonate: In cases of metabolic acidosis, sodium bicarbonate can help shift potassium into the cells.
Potassium Removal
- Diuretics: Loop diuretics like furosemide can increase the excretion of potassium in the urine.
- Dialysis: Hemodialysis is a highly effective method for rapidly removing potassium from the blood, especially in patients with renal failure.
- Potassium Binders: Oral medications such as sodium polystyrene sulfonate (Kayexalate) and newer agents like patiromer and sodium zirconium cyclosilicate can bind potassium in the gastrointestinal tract, facilitating its removal from the body.
Calcium Gluconate is the Antidote for Hyperkalemia
Mechanism of Action
Calcium gluconate is a calcium salt used to stabilize the heart in hyperkalemia. It’s the antidote for hyperkalemia. It works by antagonizing the effects of high potassium levels on cardiac myocytes, which can alter the electrical activity of the heart. By increasing the threshold potential of cardiac cells, calcium gluconate helps to reduce the excitability and risk of dangerous arrhythmias.
Administration
Calcium gluconate is typically administered intravenously. The usual dose is 10% calcium gluconate, given as a 10 mL (1 gram) infusion over 2 to 5 minutes. The effects are usually rapid, providing temporary stabilization of cardiac membranes.
Indications and Precautions
The antidote for hyperkalemia, Calcium gluconate, is indicated for patients with severe hyperkalemia, especially when ECG changes such as peaked T waves, widened QRS complexes, or sine wave patterns are present. It should be used with caution in patients with hypercalcemia or digitalis toxicity, as it can exacerbate these conditions.
Other Antidotes for High Potassium
Managing high potassium involves both immediate and long-term strategies. Immediate measures aim to prevent acute complications, while long-term strategies focus on addressing the underlying causes and preventing recurrence.
Immediate Measures
- Stabilizing the Heart: As previously discussed, calcium gluconate is crucial for stabilizing the heart.
- Shifting Potassium into Cells: Insulin with glucose, beta-2 agonists, and sodium bicarbonate are used to temporarily lower serum potassium levels.
- Enhancing Potassium Excretion: Diuretics, dialysis, and potassium binders are employed to remove excess potassium from the body.
Long-Term Strategies
- Dietary Modifications: Limiting the intake of high-potassium foods such as bananas, oranges, potatoes, and spinach can help manage potassium levels.
- Medication Adjustments: Reviewing and potentially modifying medications that contribute to hyperkalemia is essential. This may involve switching to alternative drugs or adjusting dosages.
- Monitoring and Follow-Up: Regular monitoring of potassium levels, kidney function, and overall health is necessary to detect and address any recurrence of hyperkalemia promptly.
What is the Treatment for Hyperkalemia?
Comprehensive Treatment Plan
Treating hyperkalemia involves a multi-faceted approach tailored to the severity of the condition and the patient’s overall health. The treatment plan includes:
- Initial Assessment: Evaluate the patient’s symptoms, medical history, and underlying conditions. Perform an ECG to check for cardiac effects and measure serum potassium levels.
- Immediate Interventions:
- Calcium Gluconate(Antidote for Hyperkalemia): Administer to stabilize the heart if ECG changes are present.
- Insulin and Glucose: Used to promote the intracellular shift of potassium.
- Beta-2 Agonists: Administered to help move potassium into cells.
- Sodium Bicarbonate: Consider in cases of metabolic acidosis.
- Potassium Removal:
- Diuretics: Prescribe loop diuretics to increase urinary potassium excretion.
- Dialysis: Use in severe cases, especially if renal function is impaired.
- Potassium Binders: Administer oral medications to bind potassium in the gut.
- Long-Term Management:
- Dietary Changes: Advice on a low-potassium diet.
- Medication Review: Adjust medications that may contribute to hyperkalemia.
- Regular Monitoring: Schedule regular follow-up appointments to monitor potassium levels and kidney function.
Role of Healthcare Providers
Healthcare providers play a critical role in managing hyperkalemia. They must educate patients about the condition, the importance of adhering to treatment plans, and lifestyle modifications to prevent recurrence. Providers should also stay updated on the latest guidelines and treatments to offer the best care possible.
Patiromer Treatment
Patiromer is marketed as Veltassa. It is a medication designed to treat hyperkalemia i.e. an elevated potassium level in the blood. It’s administered orally and functions by binding to potassium in your gastrointestinal tract.
Usage and Action- The drug is classified as a potassium binder and is not absorbed by the body. It exchanges calcium for potassium in the colon. Patiromer starts working within 4 to 7 hours after intake, and it’s crucial to note that it’s not intended for emergency treatment of severe hyperkalemia.
Side Effects and Considerations- Common side effects include constipation, low blood magnesium, and abdominal discomfort. Patients should be aware of the potential for hypomagnesemia (low magnesium levels) and consult their doctor if they experience symptoms like drowsiness or loss of appetite.
Remedy for Hyperkalemia
Natural and Lifestyle Remedies
While medical interventions are crucial for managing hyperkalemia, certain lifestyle and dietary changes can help prevent and control high potassium levels.
- Dietary Management:
- Low-Potassium Diet: Limit intake of high-potassium foods. Instead, focus on foods low in potassium, such as apples, berries, rice, and bread.
- Read Food Labels: Pay attention to the potassium content in packaged foods.
- Potassium Binders: If prescribed by a healthcare provider, use potassium binders as directed to help reduce potassium absorption from food.
- Hydration: Maintain adequate hydration to support kidney function and potassium excretion. However, patients with kidney disease should follow fluid intake recommendations from their healthcare provider.
- Regular Exercise: Engage in regular physical activity to support overall health and improve kidney function. Consult with a healthcare provider before starting any new exercise regimen, especially if there are existing health conditions.
- Medication Adherence: Take prescribed medications as directed. Do not adjust dosages or stop medications without consulting a healthcare provider.
Monitoring and Prevention
- Regular Check-Ups: Schedule regular visits with a healthcare provider to monitor potassium levels, kidney function, and overall health.
- Home Monitoring: Use home monitoring kits, if recommended, to check potassium levels and report any abnormalities to a healthcare provider.
- Education: Stay informed about hyperkalemia, its causes, symptoms, and management. Attend educational sessions or support groups if available.
Frequently Asked Questions, FAQs
Here are common FAQs about Hyperkalemia and Its Treatment.
1. What are the potential complications of untreated hyperkalemia?
Untreated hyperkalemia can lead to severe and potentially life-threatening complications, particularly affecting the heart. High potassium levels can disrupt the normal electrical activity of the heart, leading to arrhythmias (irregular heartbeats), which can progress to ventricular fibrillation and cardiac arrest. Other complications include muscle weakness, paralysis, and respiratory failure due to impaired muscle function.
2. How is hyperkalemia diagnosed?
Hyperkalemia is diagnosed through blood tests that measure the level of potassium in the blood. A normal potassium level ranges from 3.5 to 5.0 milliequivalents per liter (mEq/L). Levels above this range indicate hyperkalemia. Additionally, an electrocardiogram (ECG) is often performed to detect any heart abnormalities related to high potassium levels, such as peaked T waves, widened QRS complexes, and other ECG changes.
3. Can certain health conditions increase the risk of hyperkalemia?
Several health conditions can increase the risk of hyperkalemia. Chronic kidney disease (CKD) and acute kidney injury (AKI) are primary conditions that impair the kidneys’ ability to excrete potassium. Other conditions include Addison’s disease (adrenal insufficiency), type 1 diabetes (especially if poorly controlled), and conditions causing tissue breakdown (e.g., severe burns, and trauma). Additionally, metabolic acidosis and certain infections can shift potassium from cells into the bloodstream, increasing serum potassium levels.
4. What dietary changes can help manage hyperkalemia?
To manage hyperkalemia, individuals should adopt a low-potassium diet. This includes reducing the intake of high-potassium foods such as bananas, oranges, tomatoes, potatoes, spinach, and avocados. Instead, they should focus on consuming low-potassium foods like apples, berries, grapes, rice, pasta, and bread. It is also important to read food labels for hidden sources of potassium and avoid potassium-containing salt substitutes.
5. Are there any medications that can cause hyperkalemia?
Yes, several medications can contribute to hyperkalemia by either increasing potassium levels or reducing its excretion. These include:
- Angiotensin-converting enzyme (ACE) inhibitors
- Angiotensin II receptor blockers (ARBs)
- Potassium-sparing diuretics (e.g., spironolactone, eplerenone)
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Certain antibiotics (e.g., trimethoprim-sulfamethoxazole)
- Beta-blockers
Patients taking these medications should have their potassium levels monitored regularly, especially if they have underlying conditions that predispose them to hyperkalemia.
6. What role do potassium binders play in treating hyperkalemia?
Potassium binders are oral medications that help reduce the amount of potassium absorbed from the gastrointestinal tract. They bind to potassium in the intestines, forming a compound that is excreted in the stool. Common potassium binders include sodium polystyrene sulfonate (Kayexalate), patiromer (Veltassa), and sodium zirconium cyclosilicate (Lokelma). These medications are particularly useful in managing chronic hyperkalemia and preventing its recurrence.
7. How does dialysis help in treating hyperkalemia?
Dialysis is a medical procedure that filters waste products, including excess potassium, from the blood when the kidneys are unable to do so effectively. Hemodialysis involves circulating the patient’s blood through a machine equipped with a special filter (dialyzer) that removes potassium and other toxins. Dialysis is particularly effective for rapid reduction of dangerously high potassium levels, especially in patients with kidney failure or severe hyperkalemia that is unresponsive to other treatments.
8. Can exercise affect potassium levels in hyperkalemia patients?
Exercise can influence potassium levels, especially in individuals with hyperkalemia. During intense physical activity, potassium is released from muscle cells into the bloodstream. While moderate exercise is generally beneficial for overall health and kidney function, patients with hyperkalemia should consult their healthcare provider before starting any new exercise regimen. Healthcare providers can recommend appropriate exercises and monitor potassium levels to ensure safety.
9. Is there a genetic component to hyperkalemia?
While hyperkalemia itself is not typically inherited, certain genetic conditions can predispose individuals to developing it. For example, pseudohypoaldosteronism type 1 (PHA1) is a genetic disorder that affects the body’s ability to regulate potassium and sodium levels, leading to hyperkalemia. Additionally, genetic factors can influence the risk of conditions such as chronic kidney disease, which in turn can lead to hyperkalemia.
10. What lifestyle modifications can help prevent hyperkalemia?
To prevent hyperkalemia, individuals should adopt several lifestyle modifications, including:
- Following a low-potassium diet: Avoid high-potassium foods and use low-potassium alternatives.
- Staying hydrated: Adequate fluid intake supports kidney function and potassium excretion. Patients with kidney disease should follow their healthcare provider’s guidelines on fluid intake.
- Adhering to medication regimens: Take prescribed medications as directed and regularly review them with a healthcare provider to avoid drugs that increase potassium levels.
- Regular monitoring: Schedule frequent check-ups with a healthcare provider to monitor potassium levels and kidney function.
- Avoiding potassium-containing salt substitutes: Use regular salt or other seasonings that do not contain potassium.
These modifications, combined with medical management, can help you maintain safe potassium levels and prevent hyperkalemia-related complications.
Hyperkalemia is a potentially life-threatening condition that requires prompt and effective management. The antidote for hyperkalemia includes immediate interventions such as calcium gluconate to stabilize the heart, along with treatments to shift potassium into cells and enhance its excretion. Long-term management involves dietary modifications, medication adjustments, and regular monitoring.
Understanding the causes, symptoms, treatment options, and the antidote for hyperkalemia is essential for patients and healthcare providers alike. By following a comprehensive treatment plan and making necessary lifestyle changes, individuals with hyperkalemia can manage their condition effectively and reduce the risk of complications.
For those seeking more information or needing assistance with managing hyperkalemia, consulting with a healthcare provider is crucial. They can provide personalized recommendations and support to ensure optimal health and well-being.