In this segment, we will unravel what is Dyspnea?, its Causes, Symptoms, and Treatment.
Every breath you take is an intricate dance of your muscles, nerves, and organs working in perfect harmony. Yet for approximately 25% of my patients seeking medical care, this natural rhythm is disrupted by dyspnea – a complex condition that transforms the simple act of breathing into a challenging struggle.
Beyond its immediate physical impact, dyspnea serves as a crucial warning signal that demands medical attention. This condition, technically classified under ICD-10 code R06.0, manifests as more than just shortness of breath; it’s a gateway symptom that often unveils serious underlying cardiovascular and respiratory conditions requiring prompt medical intervention.
Dyspnea Definition
Approach to the patient with dyspnea refers to the medical condition characterized by shortness of breath or breathing difficulty. Patients often describe it as a sensation of not getting enough air, experiencing chest tightness, or gasping for breath. Medical professionals classify this condition under ICD-10 code R06.0, making it a standardized diagnostic term across healthcare settings.
This breathing disorder affects approximately 25% of patients seeking medical care in ambulatory settings. The significance of dyspnea extends beyond its immediate symptoms, as it often signals underlying heart or lung conditions. Healthcare providers consider this symptom essential for evaluation of dyspnea and treatment planning.
Medical Significance of Dyspnea
Dyspnea serves as a vital warning sign for numerous medical conditions, appearing in both acute and chronic presentations. As a primary symptom, it guides us as physicians through diagnostic pathways, particularly when evaluating cardiopulmonary disorders. Medical professionals recognize dyspnea’s association with respiratory distress, which can indicate severe underlying conditions that require immediate attention.
The clinical importance of dyspnea extends to patient monitoring and treatment outcomes. When patients report breathing difficulties, it often prompts healthcare providers to conduct thorough assessments, including physical examinations, diagnostic imaging, and laboratory tests. This systematic evaluation helps identify the root cause and determine appropriate treatment protocols.
Common Causes of Dyspnea
Respiratory conditions represent the primary causes of breathing difficulties, with asthma and chronic obstructive pulmonary disease frequently triggering episodes of shortness of breath. Patients with pneumonia often experience acute dyspnea due to inflammation and fluid accumulation in the lungs.
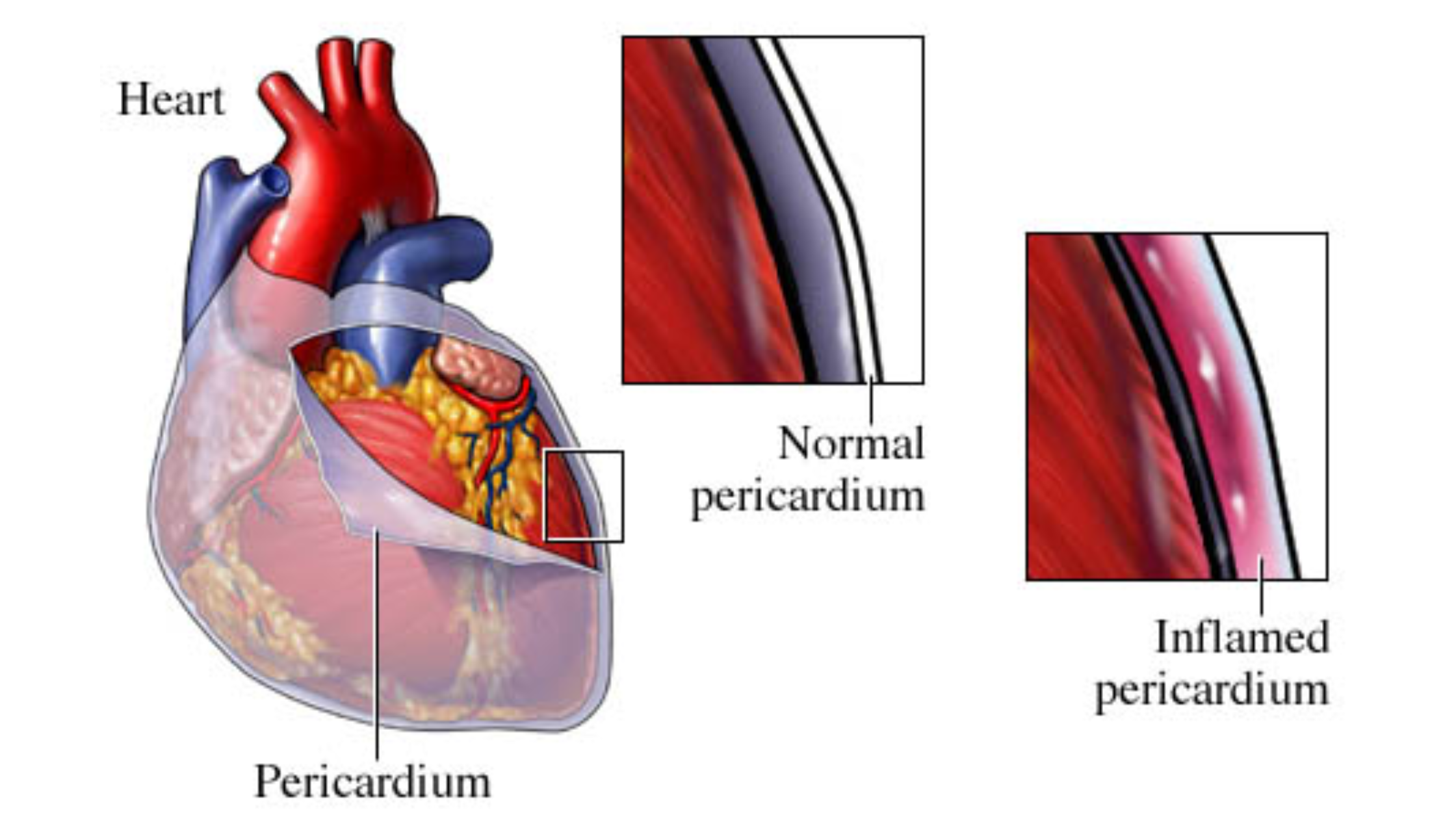
Cardiovascular disorders, particularly heart failure and myocardial infarction, lead to what medical professionals term ‘cardiac dyspnea.’ The heart’s reduced ability to pump blood effectively results in fluid buildup in the lungs, causing breathing difficulties.
Additional medical conditions like anemia limit oxygen transport throughout the body, while environmental factors such as air pollution and high altitudes can restrict normal breathing patterns. These varied causes highlight the importance of accurate medical evaluation for proper treatment.
Symptoms and Signs of Dyspnea
Patients with dyspnea typically report feeling unable to breathe deeply or get sufficient air into their lungs. The sensation often manifests as chest tightness or a feeling of suffocation. Medical observations show associated symptoms including wheezing, persistent coughing, and heart palpitations.
The psychological impact of breathing difficulties frequently leads to anxiety responses. Many patients experience panic episodes during acute dyspnea attacks, creating a cycle where anxiety worsens breathing difficulties. These symptoms can intensify during physical activity or emotional stress, prompting patients to limit their daily activities.
Patient Experience: How Dyspnea Feels
Individuals with dyspnea describe the sensation as “air hunger” – an intense need to breathe that feels unsatisfied despite effort. Patients report feeling as if they’re breathing through a straw or wearing a tight vest that restricts chest movement. The physical discomfort often creates significant emotional distress, with many patients expressing fear during breathing episodes.
This breathing difficulty affects daily activities, from climbing stairs to carrying groceries. Many patients report reducing social interactions and limiting physical activities to avoid triggering symptoms. The constant awareness of breathing patterns can lead to sleep disruption and increased fatigue, creating a cycle that impacts overall well-being.
Acute vs. Chronic Dyspnea
Medical professionals distinguish between acute and chronic breathing difficulties based on their onset and duration. Acute dyspnea appears suddenly and typically lasts hours to days, often resulting from allergic reactions, panic attacks, or respiratory infections. These episodes require prompt medical attention due to their intense nature.
Chronic dyspnea persists for weeks or months, frequently returning over time. Common underlying conditions include COPD, congestive heart failure, and obesity. While acute cases demand immediate intervention, chronic cases need ongoing management and regular medical monitoring. Understanding this distinction helps healthcare providers determine appropriate treatment strategies and assess the urgency of medical intervention.
Dyspnea on Exertion Meaning
Dyspnea on exertion (DOE) is the shortness of breath or difficulty breathing that occurs during physical activity. It is a common symptom of heart and lung conditions, such as chronic obstructive pulmonary disease (COPD), heart failure, asthma, and pulmonary hypertension. DOE happens when the body requires more oxygen during exertion, but the lungs or heart struggle to meet this demand. Common symptoms include breathlessness, chest tightness, and fatigue, which can worsen with increased activity. Treatment depends on the underlying cause and may include medications, oxygen therapy, lifestyle changes, or pulmonary rehabilitation. If dyspnea on exertion is persistent or severe, seeking medical evaluation is crucial.
Dyspnea NYHA- Classification & Severity
Dyspnea NYHA refers to the New York Heart Association (NYHA) classification of shortness of breath (dyspnea) based on heart failure severity. The NYHA functional classification categorizes dyspnea into four classes: Class I (no symptoms with normal activity), Class II (mild dyspnea with ordinary activity), Class III (marked dyspnea with minimal activity), and Class IV (severe dyspnea even at rest). This grading system helps assess heart failure progression, guide treatment decisions, and predict patient outcomes. Identifying the NYHA class of dyspnea is crucial for early intervention and improving the quality of life in heart failure patients.
Diagnostic Procedures for Dyspnea
Medical professionals begin their approach to the patient with physical examinations, noting breathing patterns and listening to lung sounds. These initial observations guide further testing requirements. Chest X-rays and CT scans show detailed images of the lungs and heart, helping identify structural abnormalities or fluid accumulation.
Pulmonary function tests, particularly spirometry, measure breathing capacity and airflow limitations. During these tests, patients breathe into specialized equipment while technicians record lung performance data. Blood work, including complete blood count and arterial blood gases, provides information about oxygen levels and potential underlying conditions such as anemia or infections.
Treatment Options for Dyspnea
Medical treatment for breathing difficulties typically begins with bronchodilators, which open airways by relaxing surrounding muscles. For acute symptoms, short-acting inhalers provide quick relief, while long-acting medications help manage chronic conditions.
Oxygen therapy plays a central role when blood oxygen levels drop below normal ranges. Patients receive supplemental oxygen through nasal cannulas or masks, improving their breathing capacity and reducing discomfort.
Approach to the patient with dyspnea combines exercise training, breathing techniques, and education to strengthen respiratory muscles and improve endurance. These programs help patients manage daily activities with less breathlessness.
We, physicians, focus on identifying and treating underlying medical conditions, such as prescribing diuretics for heart failure or antibiotics for pneumonia, to address the root cause of breathing difficulties.
Lifestyle Changes to Manage Dyspnea
Regular physical activity strengthens your respiratory muscles and improves breathing capacity. I will advise you to start with gentle exercises like walking or swimming. This allows you to build endurance gradually. Breathing exercises, including pursed-lip and diaphragmatic techniques, help control shortness of breath during daily activities.
Maintain a balanced diet and healthy weight. This will reduce strain on your respiratory system. Excess body weight creates additional pressure on the lungs, making breathing more difficult. Quitting smoking and avoiding secondhand smoke significantly improves lung function, while staying indoors during high pollution days prevents symptom triggers.
Incorporate stress management practices like meditation and progressive muscle relaxation. This helps you to reduce anxiety-related breathing difficulties. These techniques complement medical treatments and support long-term symptom management.
Preventive Measures
Approach to the patient with dyspnea plays a key role in preventing breathing difficulties. Patients with asthma or COPD benefit from following prescribed medication schedules and avoiding known triggers. Regular monitoring of lung function helps you detect changes before symptoms worsen.
Health screenings and routine check-ups allow doctors to identify potential breathing problems early. These visits include measuring blood pressure, heart rate, and oxygen levels. Patients should report any changes in breathing patterns or new symptoms during these appointments.
Environmental modifications, such as using air filters and maintaining proper humidity levels, reduce exposure to irritants. Staying current with vaccinations, particularly flu and pneumonia shots, prevents respiratory infections that can cause breathing problems.
When Should You Seek Medical Attention for Dyspnea
Medical evaluation becomes necessary when breathing difficulties occur suddenly or worsen rapidly. Patients should call emergency services if they experience severe shortness of breath accompanied by chest pain, as this combination may indicate a heart attack. The presence of blue-tinted lips or fingertips signals dangerous oxygen deprivation requiring immediate medical care.
Healthcare providers emphasize seeking prompt attention when breathing problems persist during rest or minimal physical activity. Additional warning signs include confusion, dizziness, or fainting spells related to breathing difficulties. Patients with existing respiratory conditions should contact their doctor if prescribed medications no longer control their symptoms effectively.
Impact of Dyspnea on Quality of Life
Breathing difficulties significantly affect patients’ daily routines, often restricting physical activities like climbing stairs, household chores, and exercise. Many individuals report reducing their participation in social events and family gatherings due to breathing limitations and fear of symptom onset.
The psychological toll manifests through increased rates of anxiety and depression among patients with chronic breathing problems. Sleep patterns frequently suffer, as many patients experience nighttime breathing difficulties, leading to daytime fatigue and reduced concentration.
Work performance often declines as breathing problems limit job-related tasks. Simple activities like speaking during meetings or walking between offices become challenging, affecting professional relationships and career advancement opportunities.
Patients often confuse dyspnea with orthopnea, but medical professionals note distinct differences. While dyspnea refers to general breathing difficulty, orthopnea specifically occurs when lying flat. Patients with orthopnea need to prop themselves up with pillows to breathe comfortably.
The approach to the patient includes several steps. Physicians conduct physical examinations, measuring vital signs and listening to breath sounds. Additional tests may include spirometry, blood oxygen measurements, and chest imaging. Medical professionals select tests based on symptom patterns and patient history.
Treatment methods vary according to the underlying cause. Options range from prescribed medications to breathing exercises, depending on whether the condition stems from heart, lung, or other medical issues.
Managing the Path Forward
Understanding and managing dyspnea requires a comprehensive approach that combines medical intervention with lifestyle modifications. While the condition presents significant challenges, modern medicine offers various treatment options that can substantially improve patients’ quality of life and daily functioning.
The key to successful management lies in early recognition and prompt medical attention. Through proper diagnosis, treatment adherence, and lifestyle adjustments, patients with dyspnea can regain control over their breathing and, by extension, their lives. The journey may be challenging, but with proper medical guidance and support, effective management is achievable.