Last updated on August 7th, 2024 at 02:05 pm
Living with heart failure can be daunting, but understanding the condition in depth can help you manage it better. In this comprehensive guide, I’ll take you through the symptoms, stages, treatment options, types, and causes of heart failure. We’ll also explore congestive heart failure symptoms, the ICD-10 code for heart failure, and answer some frequently asked questions.
1. Types of Heart Failure
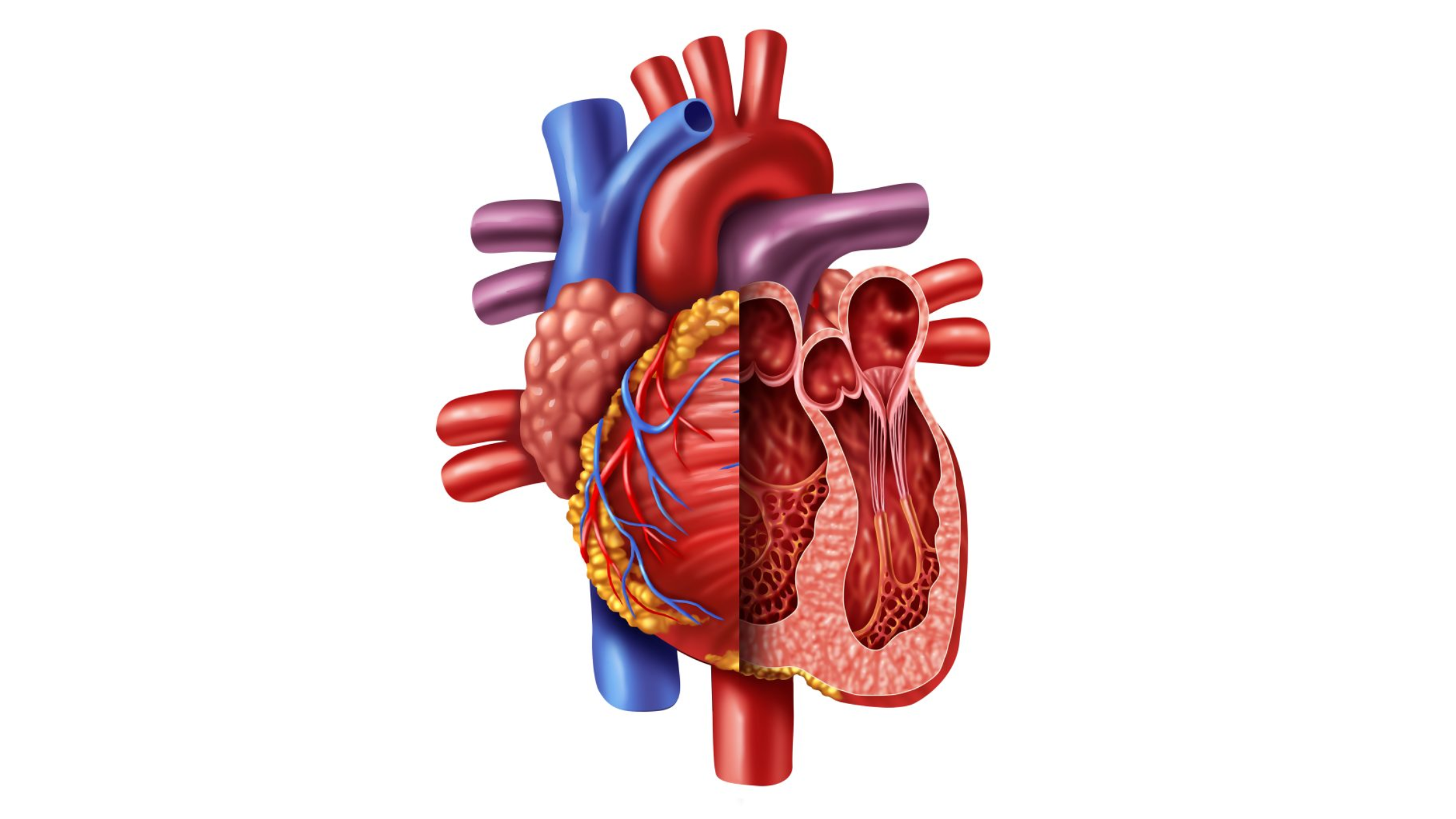
Heart failure can be classified into different types based on the area of the heart affected and how the heart’s function is compromised:
Left-Sided Heart Failure
Left-sided heart failure is the most common type and occurs when the left ventricle can’t pump blood effectively to the rest of the body. It can be further divided into:
Systolic Heart Failure: The left ventricle can’t contract forcefully enough to pump blood out to the body. This is also known as heart failure with reduced ejection fraction (HFrEF).
Diastolic Heart Failure: The left ventricle can’t relax properly, leading to inadequate filling with blood. This is also known as heart failure with preserved ejection fraction (HFpEF). (Explore left-hand side chest pain to differentiate this type of heart failure from other symptoms)
Right-Sided Heart Failure
Right-sided heart failure occurs when the right ventricle can’t pump blood effectively to the lungs. This often results from left-sided heart failure, as increased pressure in the lungs from left-sided failure puts strain on the right side. Right-sided heart failure can also result from lung diseases, such as chronic obstructive pulmonary disease (COPD) or pulmonary hypertension.
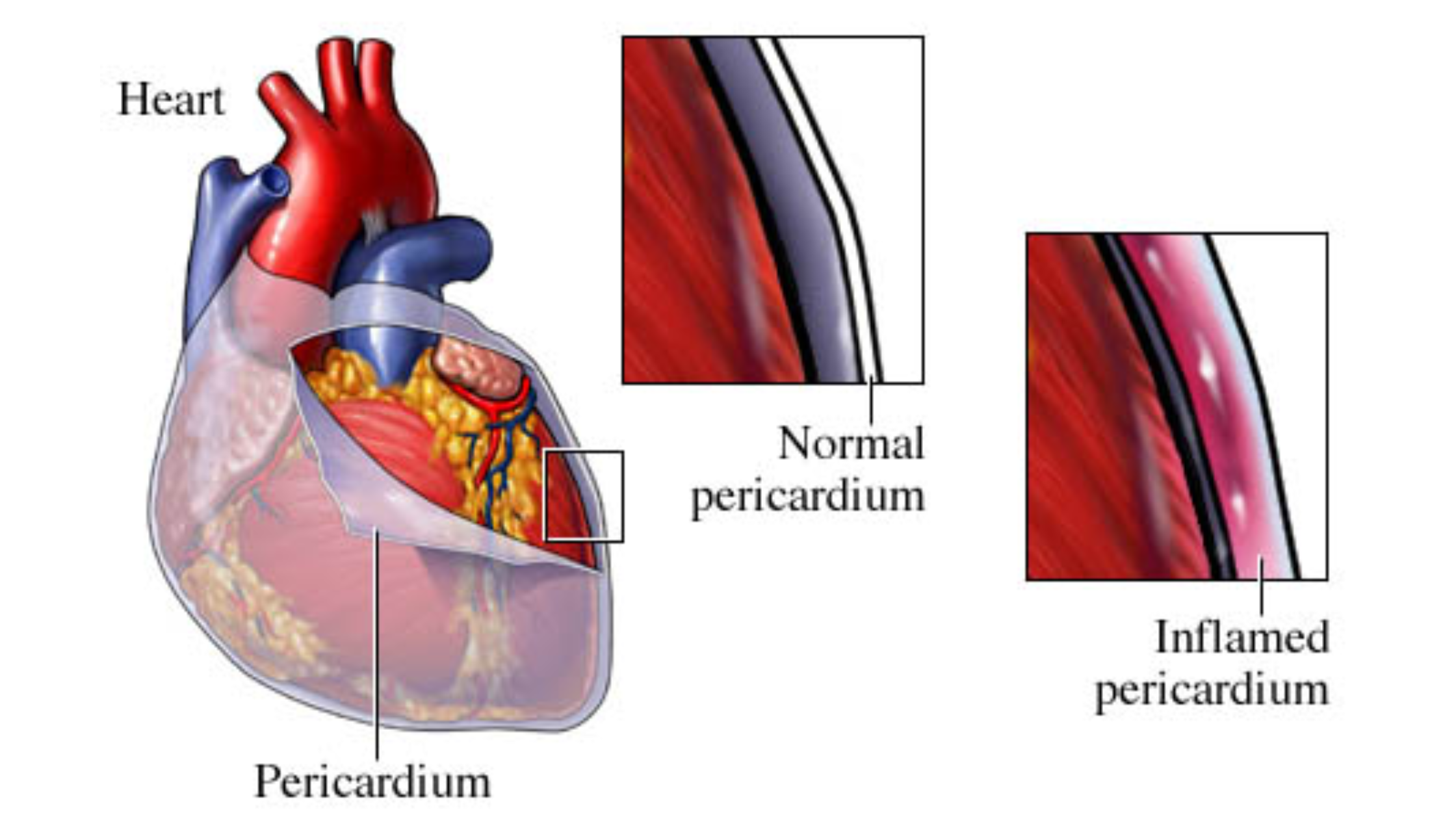
Congestive Heart Failure (CHF)
Congestive heart failure (CHF) refers to the stage where fluid builds up around the heart, causing it to pump inefficiently. It can involve both the left and right sides of the heart and leads to symptoms like swelling, shortness of breath, and fatigue.
2. Heart Failure Causes
Understanding the underlying causes of heart failure is essential for effective management and prevention. Common causes include:
Coronary Artery Disease (CAD)
CAD is the most common cause of heart failure. It occurs when the coronary arteries, which supply blood to the heart muscle, become narrowed or blocked by a buildup of fatty deposits (plaque). This reduces blood flow to the heart, leading to damage and weakening of the heart muscle.
High Blood Pressure (Hypertension)
Uncontrolled high blood pressure forces the heart to work harder to pump blood, leading to the thickening and stiffening of the heart muscle. Over time, this can weaken the heart and lead to heart failure.
Cardiomyopathy
Cardiomyopathy refers to diseases of the heart muscle that cause it to become enlarged, thickened, or stiff. This can impair the heart’s ability to pump blood effectively and lead to heart failure. Causes of cardiomyopathy include genetic factors, infections, alcohol abuse, and certain medications.
Heart Valve Problems
Malfunctioning heart valves can disrupt blood flow through the heart, causing the heart to work harder and eventually leading to heart failure. Conditions such as aortic stenosis (narrowing of the aortic valve) or mitral regurgitation (leakage of the mitral valve) are common valve problems.
Arrhythmias
Abnormal heart rhythms (arrhythmias) can cause the heart to beat too fast, too slow, or irregularly, affecting its ability to pump blood effectively. Chronic arrhythmias can weaken the heart muscle and contribute to heart failure.
Congenital Heart Defects
Structural heart defects present at birth can impair the heart’s function and lead to heart failure. These defects may involve the heart valves, walls, or blood vessels and may require surgical correction.
Other Medical Conditions
Certain medical conditions, such as diabetes, thyroid disorders, obesity, and chronic kidney disease, can increase the risk of developing heart failure. Managing these conditions through lifestyle changes and medications can help prevent heart failure.
3. Heart Failure Stages
Heart failure progresses through stages, and understanding these stages can help manage the condition more effectively. The American College of Cardiology (ACC) and the American Heart Association (AHA) classify heart failure into four stages:
Stage A: High Risk of Heart Failure
Individuals at high risk of developing heart failure but without structural heart disease or symptoms fall into Stage A. This includes those with conditions like hypertension, diabetes, metabolic syndrome, or a family history of cardiomyopathy. Management focuses on controlling risk factors through lifestyle changes and medications.
Stage B: Structural Heart Disease Without Symptoms
Stage B includes individuals with structural heart disease, such as those with a history of heart attack, valve disease, or reduced ejection fraction, but no symptoms of heart failure. Treatment at this stage aims to prevent the progression to symptomatic heart failure through medications like ACE inhibitors, beta-blockers, and lifestyle modifications.
Stage C: Structural Heart Disease With Current or Prior Symptoms
Stage C is where heart failure becomes symptomatic. Patients experience symptoms such as shortness of breath, fatigue, and fluid retention. Management includes medications, lifestyle changes, and in some cases, devices or surgery to improve heart function and alleviate symptoms.
Stage D: Advanced Heart Failure
Stage D represents advanced heart failure with severe symptoms that affect daily life despite treatment. At this stage, patients may require specialized interventions, such as mechanical circulatory support, heart transplant, or palliative care to manage symptoms and improve quality of life.
5. Heart Failure Symptoms
Recognizing the symptoms of heart failure early on is crucial for timely treatment. Here are some common symptoms to look out for:
Shortness of Breath
Shortness of breath is one of the earliest and most common symptoms of heart failure. It can occur during physical activity, such as walking or climbing stairs, or even at rest. This symptom arises because the heart can’t pump enough blood to meet the body’s needs, leading to fluid buildup in the lungs, known as pulmonary congestion.
Fatigue and Weakness
Feeling unusually tired or weak, even after minimal exertion, is another key symptom. This occurs because the heart’s reduced pumping ability means less oxygen-rich blood reaches muscles and tissues, leading to fatigue and weakness.
Swelling (Edema)
Swelling in the legs, ankles, feet, or abdomen is a sign of fluid retention, a common issue in heart failure. The kidneys, receiving less blood flow, retain fluid and sodium, which accumulates in the tissues.
Rapid or Irregular Heartbeat
A heart that beats faster than usual (tachycardia) or has an irregular rhythm (arrhythmia) can indicate heart failure. The heart tries to compensate for its reduced pumping efficiency by beating faster.
Persistent Cough or Wheezing
A persistent cough or wheezing, often accompanied by white or pink blood-tinged mucus, can occur due to fluid buildup in the lungs. This symptom, known as cardiac cough, can be mistaken for a respiratory issue but is a direct result of heart failure.
Increased Need to Urinate at Night
Frequent urination, especially at night (nocturia), is another symptom. When lying down, excess fluid retained in the tissues during the day returns to the bloodstream and is processed by the kidneys, leading to more frequent urination.
Difficulty Concentrating
Reduced blood flow to the brain can cause confusion, memory problems, and difficulty concentrating. This symptom is often overlooked but is an important indicator of heart failure.
Lack of Appetite and Nausea
Digestive issues, such as lack of appetite and nausea, can arise from reduced blood flow to the digestive system. Fluid buildup in the liver and intestines can also contribute to these symptoms.
Sudden Weight Gain
Rapid weight gain from fluid retention is a common sign of heart failure. Monitoring weight regularly can help detect this early and adjust treatment accordingly.
6. Congestive Heart Failure Symptoms
Congestive heart failure (CHF) is a specific type of heart failure characterized by the accumulation of fluid in the body’s tissues and organs. Common symptoms of CHF include:
Severe Shortness of Breath
Severe shortness of breath, particularly during physical activity or when lying flat, is a hallmark symptom of CHF. This occurs due to fluid buildup in the lungs, known as pulmonary edema.
Swelling (Edema)
Swelling in the legs, ankles, feet, and abdomen is a common symptom of CHF. This results from fluid retention caused by the heart’s reduced pumping ability.
Rapid Weight Gain
Rapid weight gain from fluid retention is a key indicator of worsening CHF. Monitoring weight daily can help detect fluid buildup early and adjust treatment accordingly.
Persistent Cough or Wheezing
A persistent cough or wheezing, often accompanied by frothy or pink-tinged sputum, is a symptom of CHF. This occurs due to fluid congestion in the lungs.
Fatigue and Weakness
Fatigue and weakness, even with minimal exertion, are common symptoms of CHF. Reduced blood flow to the muscles and tissues leads to these symptoms.
Loss of Appetite and Nausea
Digestive issues, such as loss of appetite and nausea, can occur in CHF due to fluid buildup in the liver and intestines. This can also lead to early satiety and unintentional weight loss.
Difficulty Sleeping
Difficulty sleeping, particularly when lying flat, is common in CHF. Many patients find relief by sleeping with the head elevated or using multiple pillows to reduce shortness of breath.
7. Heart Failure Treatment
Treating heart failure involves a combination of lifestyle changes, medications, and sometimes surgical interventions. The goal is to improve symptoms, slow disease progression, and enhance quality of life.
Lifestyle Changes
Implementing healthy lifestyle changes is crucial for managing heart failure. These changes can significantly impact the progression of the disease and improve overall well-being.
Diet: Adopting a heart-healthy diet is essential. This includes reducing sodium intake to prevent fluid retention, eating plenty of fruits and vegetables, whole grains, lean proteins, and limiting saturated fats and cholesterol. The DASH (Dietary Approaches to Stop Hypertension) diet is often recommended.
Exercise: Regular physical activity tailored to your ability helps improve cardiovascular health, reduce symptoms, and enhance quality of life. Exercise programs should be designed with a healthcare provider to ensure they are safe and effective.
Weight Management: Maintaining a healthy weight reduces the strain on the heart. Monitoring weight daily helps detect fluid retention early, allowing for timely adjustments in treatment.
Smoking Cessation: Quitting smoking is crucial for heart health. Smoking damages blood vessels, reduces oxygen supply, and increases the risk of coronary artery disease, a leading cause of heart failure.
Limiting Alcohol: Reducing or eliminating alcohol intake is important, as excessive alcohol can weaken the heart muscle and exacerbate heart failure symptoms.
Medications
Various medications are used to manage heart failure, targeting different aspects of the condition:
ACE Inhibitors: These medications help relax blood vessels, reduce blood pressure, and decrease the heart’s workload by blocking the production of angiotensin II, a substance that narrows blood vessels.
Beta-Blockers: Beta-blockers reduce heart rate and blood pressure, improving heart function and reducing symptoms. They also help prevent arrhythmias and reduce the risk of sudden cardiac death.
Diuretics: Diuretics, or water pills, help remove excess fluid from the body, reducing swelling and easing the workload on the heart. Common diuretics include furosemide and spironolactone.
Aldosterone Antagonists: These medications help reduce fluid retention and improve heart function by blocking the effects of aldosterone, a hormone that causes fluid retention.
Digoxin: Digoxin helps strengthen the heart muscle and regulate heart rhythm. It is often used in patients with severe symptoms or atrial fibrillation.
Surgical Options
In some cases, surgical interventions may be necessary to treat underlying causes of heart failure or improve heart function:
Coronary Bypass Surgery: This surgery improves blood flow to the heart by creating new pathways around blocked coronary arteries.
Heart Valve Repair or Replacement: Addressing valve problems can improve blood flow through the heart and reduce symptoms of heart failure.
Implantable Cardioverter-Defibrillators (ICDs): ICDs help regulate heart rhythm and prevent sudden cardiac death in patients with severe arrhythmias.
Left Ventricular Assist Devices (LVADs): LVADs help the heart pump blood and are used in patients with advanced heart failure who are awaiting a heart transplant or are not candidates for transplant.
Heart Transplant: In severe cases where other treatments have failed, a heart transplant may be considered. This involves replacing the diseased heart with a healthy donor heart.
8. Heart Failure ICD-10
The ICD-10 code for heart failure is a medical classification used for diagnosing and billing purposes. The primary codes for heart failure include:
- I50.1: Left ventricular failure
- I50.2: Systolic (congestive) heart failure
- I50.3: Diastolic (congestive) heart failure
- I50.4: Combined systolic and diastolic heart failure
- I50.9: Heart failure, unspecified
These codes help healthcare providers document and track the condition accurately, ensuring appropriate treatment and reimbursement.
9. Heart Failure Frequently Asked Questions (FAQs)
What are the first signs of heart failure?
The first signs of heart failure often include shortness of breath, fatigue, and swelling in the legs, ankles, or feet. Other early symptoms may include rapid or irregular heartbeat, persistent cough or wheezing, and increased need to urinate at night.
Can heart failure be reversed?
While heart failure cannot be completely reversed, its progression can be slowed, and symptoms can be managed effectively through lifestyle changes, medications, and, in some cases, surgical interventions. Early diagnosis and treatment are crucial for improving outcomes.
How is heart failure diagnosed?
Heart failure is diagnosed through a combination of medical history, physical examination, and diagnostic tests. Common tests include blood tests, chest X-rays, electrocardiograms (ECGs), echocardiograms, stress tests, and cardiac MRI or CT scans.
What is the life expectancy of someone with heart failure?
The life expectancy of someone with heart failure varies based on the severity of the condition, the individual’s overall health, and how well they manage their symptoms and underlying causes. With proper treatment and lifestyle changes, many people with heart failure can live fulfilling lives for many years.
How can I prevent heart failure?
Preventing heart failure involves managing risk factors such as high blood pressure, diabetes, and coronary artery disease. Adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, maintaining a healthy weight, not smoking, and limiting alcohol intake, can significantly reduce the risk of heart failure.
In Summary
Understanding heart failure, its symptoms, stages, treatment options, types, and causes, is essential for effective management and improved quality of life. By recognizing the early signs, making necessary lifestyle changes, and following prescribed treatments, individuals with heart failure can lead fulfilling lives. If you suspect you have symptoms of heart failure or are at risk, consult with a healthcare provider for proper diagnosis and management.


Your article helped me a lot, is there any more related content? Thanks!